Case Study No 82
A 50-year-old female patient with a previous history of sarcomatoid bladder cancer underwent radical cystectomy (pT3a, pN0, cM0, R0) in 2007 with the construction of an ileal conduit. She now presents with a chronic inflammation of the stoma.
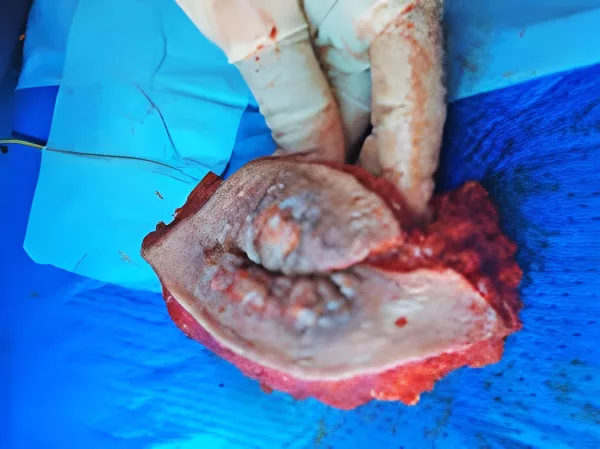
This started in 2012 with severe and symptomatic peristomal skin changes (Fig. 1) without any evidence of disease recurrence. A variety of treatments were applied by stomatherapy (e.g., burn/silver nitrate, creams, plates, herbal medicines, and egg whites).
In 2014, biopsies showed fibrous and inflammatory changes without atypia. She was then treated by a dermatologist and received local corticoids. None of this worked.
In 2017, another biopsy was done with the same result as in 2014. Microbiology was also negative.
Discussion points:
- Are further investigations required?
- What management is appropriate?
Case 82 continued
We started by measuring the length of Bricker´s loop (12 cm) to plan the possibility of using the same loop to create a new cutaneous stoma after removing the affected area.
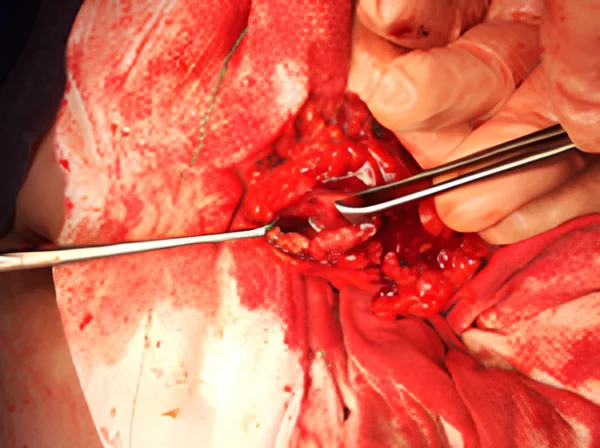
The patient underwent surgery with the removal of the affected stoma. Histology showed fibrous and inflammatory tissue without malignancy (Fig. 2).
Fig. 3 shows the release and mobilisation of the loop next to the aponeurosis, gaining approximately 3 cm in length to create a new stoma.
We then performed an abdominoplasty with the reduction of the abdominal adipose tissue so that the length of the loop could reach the new stoma in healthy skin (Fig. 4).
Fig. 5 shows the post-operative result six years later.
Commentary on Case 82
By Prof. Dr. Axel Heidenreich, University Hospital Cologne, Germany
The patient is suffering from significant peristomal inflammation despite several local conservative treatment approaches. Upon closer inspection, it becomes evident that:
- Hyperplastic, papillomatous skin lesions have developed;
- No appropriate eversion of the aboral ileum segment has been performed;
- There is a retraction of the stoma;
- There is bulging of the peristomal area, which might resemble a parastomal hernia.
Are additional imaging studies indicated?
Looking at the image with a patient in a supine position, it is difficult to diagnose a parastomal hernia. If there is evidence of such a hernia during physical examination of the patient in a standing position, I would schedule a CT scan to have an idea about the extent and the content of such a hernia.
If there is no evidence of a parastomal hernia during physical examination, the ileal conduit needs to be examined. The retraction of the stoma can be due to malvascularization of the ileum due to extensive tension on the mesentery at the time of initial surgery resulting in scarring, or an inadequately performed eversion of the ileum segment at the time of the primary surgery.
These two options need to be differentiated since they result in different treatment strategies. I recommend performing a loopogram of the conduit wherein the scarring will be identified by a small-caliber, straight ileum. Furthermore, the loopogram will give information about the length of the ileum conduit and any anatomic abnormalities.
Which treatment should be offered?
The hyperplastic papillomatous skin lesions are the result of chronic exposure of the skin to urine, referred to as urea dermatitis. There is no option for conservative treatment, which will give satisfactory results. For me, redoing the surgery is the only way to solve the problem. The surgical approach depends on the various findings outlined above, such as:
Failed eversion
This approach involves the excision of the skin around the skin lesions; complete mobilisation of the conduit through the subcutis, the fascia and the rectus abdominis muscle and eversion of the ileal segment with resorbable sutures. Sometimes this approach can be done without the transperitoneal approach, but sometimes the peritoneal cavity must be opened.
Malvascularisation
In this approach, the ileum conduit has to be redone with complete resection of the ileal segment from the skin to the ureterointestinal anastomoses, and construction of a new ileum conduit.
Parastomal hernia
This is the most difficult procedure since the long-term results are usually imperfect. Surgery should include the principles of the failed eversion approach and additionally either mesh implants or transpositioning of the stoma to the contralateral side.
Commentary on Case No. 82 – Chronic peristomal inflammation following ileal conduit urinary diversion
By Prof. Morgan Rouprêt, Urologie, Hôpital Pitié-Salpétrière, APHP Sorbonne Université (FR)
This is a challenging and instructive case of a 50-year-old woman with a history of sarcomatoid variant bladder cancer, treated by radical cystectomy and ileal conduit (Bricker) in 2007, now presenting with chronic peristomal inflammation. The persistent nature of her symptoms, which began after five years and the failure of multiple conservative treatments highlight the complexity of long-term stoma care in patients with urinary diversions.
The timeline reveals progressive and treatment-refractory skin inflammation since 2012. A comprehensive conservative approach was used, including burn/nitrate solutions, barrier creams, herbal applications and even egg whites. Dermatologic referral led to topical corticosteroid therapy. Repeated biopsies in 2014 and 2017 demonstrated only fibrous and inflammatory changes, without evidence of dysplasia or malignancy. Microbiological assessments were negative. The absence of disease recurrence and negative histology are reassuring, but the persistent nature of symptoms raises concern for a structural or mechanical complication at the stoma site.
At this stage, I would argue that additional conservative management is unlikely to succeed. The patient has already undergone an extensive therapeutic algorithm, and there is no new dermatologic or infectious pathology to address. The chronicity, location and resistance to medical management suggest that the inflammation may be due to local mechanical irritation, ischemia or even occult low-grade infection within the conduit or at the skin-conduit interface. Poor appliance fit, mucocutaneous separation or stomal retraction can lead to chronic skin breakdown and inflammation, particularly in long-standing diversions.
In such cases, surgical revision should be considered. I would propose a resection of the diseased stoma and the construction of a new ileal conduit, ideally in a different abdominal quadrant if feasible. This approach has been described and validated in similar clinical situations and may offer the only route to durable symptom resolution and improved quality of life (Lardeux et al., Progrès en Urologie, 2023).
While surgical revision carries inherent risks, particularly in a patient with prior major pelvic surgery, it remains a definitive option when all conservative measures have failed and quality of life is severely impaired. A multidisciplinary evaluation including urology, stomatherapy and possibly plastic surgery may assist in optimising outcomes.
In conclusion, this case underscores the importance of ongoing follow-up in patients with urinary diversions and the potential need for surgical re-intervention years after the initial procedure when conservative approaches prove inadequate.