Late onset hypogonadism (LOH), what does that mean for a man?
Hypogonadism is a condition many men experience as they age. Testosterone levels naturally decline over time, and this decrease can lead to significant health and quality of life (QoL) issues. Signs of low hypogonadism are erectile dysfunction (ED), loss of morning erections and lower libido. In this article, we will describe the problem, complaints, causes and treatment options.
What is LOH, and epidemiology
LOH is also called ‘adult male hypogonadism’. The definition from the EAU Guidelines tells us this: Male hypogonadism is a clinical syndrome which comprises of symptoms with or without signs and biochemical evidence of testosterone deficiency.
The main symptoms are a decrease of erectile function and morning erections, and a decrease of libido. Besides this, multiple organ functions can be influenced by lower testosterone levels in men affecting the QoL.
The prevalence increases with age because of lower levels of testosterone in the blood due to co-morbidities. The incidence of LOH accounts for a small percentage of total hypogonadism. More men are consulting a doctor thinking they have a low testosterone level. In men aged 40-79 years, the incidence of symptomatic hypogonadism varies between 2.1 and 5.7%.
According to the classification of LOH, it must comprise both persistent specific symptoms of ED and low libido and biochemical evidence of testosterone deficiency. Several drugs can also induce the testosterone level such as methotrexate, chemotherapy agents, and testosterone synthesis inhibitors like ketoconazole. Androgens resistance or decreased bioactivity can be caused by 5α reductase inhibitors, spironolactone. Drug induced oestrogen receptor blockades by clomiphene and tamoxifen. Of cause, other conditions like testicular diseases or orchiectomy can also induce hypogonadism.
The prevalence in men with type 2 diabetes (T2DM), metabolic syndrome, obesity and cardiovascular diseases is higher. Impaired glucose tolerance can be influenced negatively by low testosterone levels. A large study showed that testosterone therapy in men with testosterone level of <14 nmol/l reduced the proportion of patients with T2DM for two years.
The large European Male Aging Study (EMAS) showed a decline of testosterone level of 0.4% per year in TT and 1.3% in free testosterone. The Massachusetts Male Aging Study (MMAS) combined data and showed that associated comorbidity and obesity significantly decreased total and free testosterone. This leads to the concept op functional hypogonadism where testosterone treatment is discussed.
Diagnosis of LOH
The main approach to diagnosing hypogonadism involves a thorough history review of the patient, including sexual history, physical symptoms and psychological symptoms. Physical examination and laboratory diagnostics are also included. Obesity is frequently associated with LOH, the waist circumference and BMI should be measured.
To start, you can first determine TT. If decreased you can take a compete laboratory diagnostics with Luteinising hormone, TT, (calculated) free testosterone, Sex Hormone Binding Globulin (SHBG), PSA, glucose, lipids. Due to its negative influence on libido, prolactin can also be considered as first-line screening in patients with reduced sexual desire.
With increasing SHBG, the free testosterone decreases even more in comparison to the TT. Elevated SHBG can result from medication, hyperthyroidism, liver disease, ageing, smoking and HIV infection.
A testosterone level of < 12 nmol/l is a reliable threshold to diagnose LOH together with signs and symptoms of ED and libido loss. A calculated free testosterone of < 220 pmol/l can be suggested as cut off point as recommended by the EAU Guideline on sexual health. The testosterone level should be measured between 7.00 and 11.00 in the morning, preferably fasting. It should be repeated on two sperate occasions any time in between. Prolactin should be measured with suspicion of secondary hypogonadism and/or low sexual desire.
Before starting testosterone replacement therapy, try to safely eliminate drugs that can interfere with hypothalamic-pituitary axis. Rule out any existing prostate cancer as this is accounted for as a contraindication. Another contraindication is high haematocrit of >54% as testosterone therapy can increase haematocrit even more. Men with COPD and OSAS are associated with an increased risk as well.
Treatment of LOH
LOH can be treated with testosterone replacement therapy (TRT). Different modalities are available like gels and injectables. Besides this, lifestyle changes and weight loss in obesity men should be discussed with the patient as a first step to treat LOH and increase the testosterone level. A meta-analysis showed that a low-calorie diet can restore TT and free testosterone levels by reducing the oestrogen in the body by visceral fat loss. This restores the normal gonadotropin circulating levels. This can be reached by increasing the physical activity. Besides this, men can benefit more from combination of lifestyle change with TRT if symptomatic hypogonadal.
Injectable testosterone is available based on half-lives. Short acting formulas has the disadvantage of wide fluctuation in plasma testosterone levels and therefore often unpleasant for patients. Long lasting formulation of injectable testosterone allows the maintenance of a stable testosterone level with a ten to fourteen weeks frequency. This depending on the therapeutic range of 12-18 nmol/l.
Transdermal testosterone formulations, gel is the most frequently used application. It is applied on daily basis every morning and quickly absorbed in the subcutaneous tissue. It will be released over 24 hours. Local skin adverse effects are limited. It allows transfer of Testosterone if the skin is not covered by clothing or apply on skin which is not often touched by others. Several brands of testosterone gels are available in the European countries, mostly in pump bottle or sachets. The regular dosage is 40-50 mg per day.
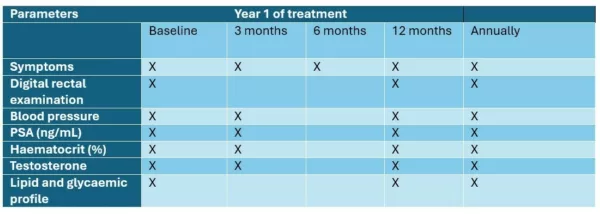
The follow up of patients on TRT is described in the EAU Guideline on male sexual dysfunction. See below table.
Special consideration is required for patients with comorbidities. Men actively trying to conceive should not undergo TRT, as it is contraindicated. This impairs the spermatogenesis and sperm maturation through inhibition of the gonadotropin secretion of FSH. Male breast cancer is an absolute contraindication for TRT since testosterone influences the development of breast cancer by its conversion to oestrogen.
Effect of TRT on erectile function is the most common reason to start TRT. A meta-analysis showed that men with more severe testosterone deficiency (<8 nmol/l) experience more improvement on sexual function than men with mild hypogonadism (<12 nmol/l). The TRAVERSE study showed that hypogonadal men with pre-existing or high risk of cardiovascular disease did not experience better erectile dysfunction after two years of TRT. In more severe erectile dysfunction phosphodiesterase type 5 inhibitors can be advised in combination with TRT.
Other positive effects of TRT can be improvement of vitality and physical strength, mood and cognition. The evidence on these aspects is weak. (RL) The influence on body composition and metabolic function is also limited. However, the influence on osteoporosis and bone mineral density with very low TT levels of < 3.5 nmol/l is more pronounce and independent from age. But the risk of bone and hip fractures did not decrease.
Conclusion
LOH is a testosterone deficiency in men which mostly starts in adulthood or old age, not associated with congenital conditions or acquired by i.e. orchiectomy. A TT of < 8 nmol/l is defined as an absolute testosterone deficiency, whereas level of 8-12 nmol/l and free testosterone of < 220 nmol/l is defined as hypogonadism. Often a higher level of luteinising hormone is seen in these men. The testosterone in the blood should be measured between 7.00 and 11.00 AM, fasting. Testosterone treatment is advised in hypogonadal men with erectile dysfunction and can be combined with phosphodiesterase type 5 inhibitors. Besides this, it is advised to improve lifestyle and reduce weight. Use testosterone gels or long-lasting depot administration to treat testosterone deficiency. Counsel and follow up on men treated with TRT according to the recommended follow up scheme.
Literature/references
- Salonia A, Bettoocchi C, Carvalho J, et al. Guidelines on sexual and reproductive health. EAU;2025. pp.3-33.
- Yassin, A., et al. Testosterone Therapy in Men with Hypogonadism Prevents Progression From Prediabetes to Type 2 Diabetes: Eight-Year Data From a Registry Study. Diabetes Care, 2019. 42: 1104. https://www.ncbi.nlm.nih.gov/pubmed/30862651
- Wu, F.C., et al. Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab, 2008. 93: 2737. https://www.ncbi.nlm.nih.gov/pubmed/18270261
- Mohr, B.A., et al. Normal, bound and nonbound testosterone levels in normally ageing men: results from the Massachusetts Male Ageing Study. Clin Endocrinol (Oxf), 2005. 62: 64. https://www.ncbi.nlm.nih.gov/pubmed/15638872
- Corona, G., et al. Body weight loss reverts obesity-associated hypogonadotropic hypogonadism: a systematic review and meta-analysis. Eur J Endocrinol, 2013. 168: 829. https://www.ncbi.nlm.nih.gov/pubmed/23482592
- Corona, G., et al. Treatment of Functional Hypogonadism Besides Pharmacological Substitution. World J Mens Health, 2020. 38: 256. https://www.ncbi.nlm.nih.gov/pubmed/31496147
- Corona, G., et al. The pharmacotherapy of male hypogonadism besides androgens. Expert Opin Pharmacother, 2015. 16: 369. https://www.ncbi.nlm.nih.gov/pubmed/25523084
- Isidori, A.M., et al. Outcomes of androgen replacement therapy in adult male hypogonadism: recommendations from the Italian society of endocrinology. J Endocrinol Invest, 2015. 38: 103. https://www.ncbi.nlm.nih.gov/pubmed/25384570
- Corona, G., et al. Meta-analysis of Results of Testosterone Therapy on Sexual Function Based on International Index of Erectile Function Scores. Eur Urol, 2017. 72: 1000. https://www.ncbi.nlm.nih.gov/pubmed/28434676
- Pencina, K.M., et al. Effect of Testosterone Replacement Therapy on Sexual Function and Hypogonadal Symptoms in Men with Hypogonadism. J Clin Endocrinol Metab, 2024. 109: 569. https://www.ncbi.nlm.nih.gov/pubmed/37589949