Mapping the burden of female urinary incontinence: Prevalence, risk factors, and economic impact
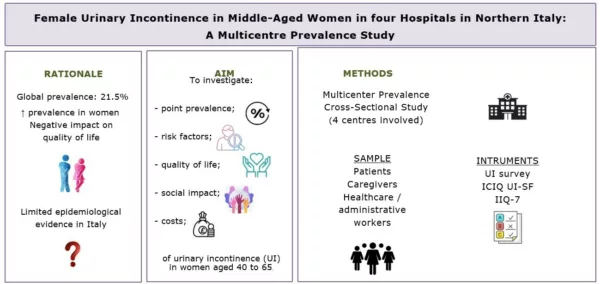
This article summarises and discusses the findings of the study by Trapani, Villa, Marcomini et al. (2025) recently published in the International Journal of Urological Nursing titled “Prevalence, Risk Factors and Costs of Female Urinary Incontinence: A Multicentre Cross-Sectional Study.”
Urinary incontinence (UI) is one of the most frequent chronic conditions affecting women worldwide. Although it is not a life-threatening disorder, its consequences extend far beyond physical discomfort, affecting emotional health, social relationships, sexual function and overall quality of life (1). The global prevalence of UI is estimated at over 20% of the adult population, with women representing the vast majority of cases (2). Despite this, embarrassment and stigma often lead to underreporting, delaying diagnosis and treatment (3).
In Italy, the most recent national data on UI prevalence and risk factors are outdated, and information about its economic impact remains limited (4). Recognising this gap, a research team from the IRCCS San Raffaele Hospital and Vita-Salute San Raffaele University conducted a multicentre study to assess how common UI is among middle-aged women, to identify key risk factors, and to quantify the direct costs associated with its management. The findings offer valuable insights for nursing and midwifery practice, where preventive and educational interventions can play a central role.
Study methods
This cross-sectional study was carried out in four hospitals located in Northern Italy. The research design followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines and complied with the Declaration of Helsinki and Good Clinical Practice principles. Ethical approval was granted by the Territorial Ethics Committee (CET 29-2024), and all participants provided written informed consent. The study protocol was registered on ClinicalTrials.gov (NCT06291441).
A total of 722 women aged between 40 and 65 years took part in the survey. Participants included both outpatients and hospital staff, recruited through convenience sampling. Pregnant and postpartum women were excluded. Data were collected via a structured paper questionnaire, which gathered socio-demographic details, lifestyle information, comorbidities, and gynaecological and obstetric history. Respondents also reported any weekly expenses related to incontinence management, such as pads, medical visits or medications.
To assess the presence and severity of urinary incontinence, the International Consultation on Incontinence Questionnaire – Urinary Incontinence Short Form (ICIQ-UI SF) was used. This validated instrument evaluates frequency and amount of leakage, its impact on quality of life, and the type of incontinence (stress, urgency, or mixed). Scores range from 0 to 21 and are classified as mild, moderate, severe or very severe.
Data analysis combined descriptive and inferential statistics. Logistic regression models identified predictors of UI occurrence, subtype and severity, while Pearson’s correlation was used to explore the association between incontinence severity and healthcare costs. Statistical significance was set at p < 0.05.
Results
The average age of the 722 respondents was 52.6 years. The large majority were Italian citizens, and most had completed secondary education. The overall prevalence of urinary incontinence in this population was 44.8%, meaning that nearly one in two middle-aged women experienced some degree of leakage. Stress urinary incontinence (SUI) was the most common subtype, affecting 39.1% of respondents, followed by urgency urinary incontinence (UUI) in 13.8% and mixed urinary incontinence (MUI) in 9.1%. In terms of severity, 19.6% of participants reported mild symptoms, 20.4% moderate symptoms, and 4.3% severe or very severe leakage.
The multivariate analysis revealed several important risk factors (Table 1). Higher body mass index (BMI), hypertension, multiple vaginal deliveries, bladder emptying difficulties, depression, and smoking were all significantly associated with UI. Specific patterns emerged for different subtypes: SUI was mainly linked to increased BMI, constipation and pelvic organ prolapse, while UUI and MUI were more strongly associated with hypertension and smoking, suggesting distinct pathophysiological mechanisms. Interestingly, older age of the participant’s children appeared to be a protective factor, possibly reflecting gradual recovery of pelvic floor muscle tone over time.
From an economic standpoint, the study found that most women (54.6%) reported no direct weekly costs for incontinence management, whereas 26.8% spent less than €3 per week and 11.6% up to €5. Only a small fraction of participants incurred expenses above €10 weekly. Nevertheless, there was a significant positive correlation between incontinence severity and total weekly expenditure (r = 0.480, p < 0.001). Women with severe or very severe leakage spent more on absorbent products and healthcare services, confirming that urinary incontinence is associated with a measurable economic burden even at the individual level.
Discussion
The results of this multicentre study position Northern Italy within the higher range of international prevalence estimates for female urinary incontinence. Compared with previous Italian studies from the early 2000s (5) , the observed prevalence appears to have increased. This may reflect both a true rise - linked to lifestyle factors such as obesity, reduced physical activity, and chronic diseases - and a greater willingness among women to disclose symptoms due to growing awareness and reduced stigma (6) .
The identification of modifiable risk factors such as hypertension, smoking, overweight and depression has major clinical implications. Hypertension emerged as a strong predictor, particularly for urgency and mixed incontinence, suggesting that vascular dysfunction may contribute to detrusor instability.
Similarly, elevated BMI was significantly associated with stress incontinence, confirming the role of mechanical pressure on pelvic structures. Multiple vaginal deliveries, already recognised in the literature as a major risk factor, were again shown to increase the likelihood and severity of UI across all subtypes. The association between depression and severe leakage deserves special attention. Psychological distress may amplify the perception of urinary symptoms, reduce adherence to behavioural therapies, and limit help-seeking behaviour. Integrating psychological screening and counselling within urogynecological and nursing care pathways may therefore enhance overall management.
In addition to its clinical relevance, this study sheds light on the economic dimension of UI. The observed relationship between symptom severity and direct costs supports the argument that early intervention could be cost-effective. Even modest weekly expenses translate into substantial annual figures at the population level. Considering that nearly half of middle-aged women experience some form of leakage, preventive measures could significantly reduce both personal and healthcare system expenditures.
From a professional perspective, the findings call for a stronger role of nurses and midwives in early detection, education, and prevention. Counselling on pelvic floor exercises, weight management, and modifiable risk factors should be integrated into routine health assessments, especially for women with hypertension, depression, or a history of multiple vaginal births. Addressing UI proactively may prevent the progression from mild to severe forms, thereby improving quality of life and reducing costs.
Conclusions
Urinary incontinence affects almost one out of every two middle-aged women in Northern Italy and remains a major yet underestimated public health issue. The study highlights a complex interaction of biological, behavioural and psychosocial factors underlying its development. Many of these determinants - including obesity, smoking and hypertension - are preventable or manageable through lifestyle modification and education.
For healthcare professionals, these findings reinforce the need for a multidisciplinary, patient-centred approach. Nurses, midwives and physicians should work together to identify at-risk women, promote pelvic floor health, and encourage open discussion to overcome the persistent stigma associated with urinary incontinence. Reducing the prevalence and severity of UI is not only a matter of comfort or dignity but also of economic sustainability and gender-specific health equity.
References
(1) S. Batmani, R. Jalali, M. Mohammadi, and S. Bokaee, “Prevalence and Factors Related to Urinary Incontinence in Older Adults Women Worldwide: A Comprehensive Systematic Review and Meta- Analysis of Observational Studies,” BMC Geriatrics 21, no. 1 (2021): 212, https:// doi. org/ 10. 1186/ s1287 7- 021- 02135 - 8.
(2) D. E. Irwin, Z. S. Kopp, B. Agatep, I. Milsom, and P. Abrams, “Worldwide Prevalence Estimates of Lower Urinary Tract Symptoms, Overactive Bladder, Urinary Incontinence and Bladder Outlet Obstruc tion,” BJU International 108, no. 7 (2011): 1132–1138, https:// doi. org/ 10. 1111/j. 1464- 410X. 2010. 09993. x. 11. I.
I.Milsom and M. Gyhagen, “The Prevalence of Urinary Inconti nence,” Climacteric 22, no. 3 (2019): 217–222, https:// doi. org/ 10. 1080/ 13697 137. 2018. 1543263.
A.K. Nambiar, S. Arlandis, K. Bø, et al., “European Association of Urology Guidelines on the Diagnosis and Management of Female Non- Neurogenic Lower Urinary Tract Symptoms. Part 1: Diagnostics, Overactive Bladder, Stress Urinary Incontinence, and Mixed Urinary Incontinence,” European Urology 82, no. 1 (2022): 49–59, https:// doi. org/ 10. 1016/j. eururo. 2022. 01. 045.
(3) L. P. Chisholm, E. M. Sebesta, S. Gleicher, M. Kaufman, R. R. Dmo chowski, and W. S. Reynolds, “The Burdens of Incontinence: Quantify ing Incontinence Product Usage and Costs in Women,” Neurourology and Urodynamics 41, no. 7 (2022): 1601–1611, https:// doi. org/ 10. 1002/ nau. 25007.
C. Murphy, M. Avery, M. Macaulay, and M. Fader, “Experiences and Impact of Living With Incontinence Associated Stigma: A Protocol for a Systematic Review and Narrative Synthesis of Qualitative Studies,” PLoS One 17, no. 7 (2022): e0270885, https:// doi. org/ 10. 1371/ journ al. pone. 0270885.
(4-6) M. Monti, M. Fischetti, G. Santangelo, et al., “Urinary Incontinence in Women: State of the Art and Medical Treatment,” Minerva Obstet rics and Gynecology 73, no. 2 (2021): 135–139, https:// doi. org/ 10. 23736/ S2724 - 606X. 20. 04635 - 3.
R. Alvaro, F. Araco, G. Gravante, et al., “Epidemiological Aspects of Urinary Incontinence in a Female Population of an Italian Region,” International Urogynecology Journal 21, no. 7 (2010): 873–883, https:// doi. org/ 10. 1007/ s0019 2- 010- 1112- 6.
A. Bortolotti, B. Bernardini, E. Colli, et al., “Prevalence and Risk Factors for Urinary Incontinence in Italy,” European Urology 37, no. 1 (2000): 30–35, https:// doi. org/ 10. 1159/ 00002 0096.
F. Parazzini, M. Lavezzari, and W. Arbitani, “Prevalence of Overac tive Bladder and Urinary Incontinence,” Journal of Family Practice 51, no. 12 (2002): 1072–1075.
S. Siracusano, R. Pregazzi, G. d'Aloia, et al., “Prevalence of Urinary Incontinence in Young and Middle- Aged Women in an Italian Urban Area,” European Journal of Obstetrics & Gynecology and Reproduc tive Biology 107, no. 2 (2003): 201–204, https:// doi. org/ 10. 1016/ S0301 - 2115(02) 00407 - 4. 21. K. Avery, J. Donov