4. PATHOLOGICAL STAGING, GRADING AND CLASSIFICATION SYSTEMS
4.1. Definition of non-muscle-invasive bladder cancer
Urothelial tumours confined to the mucosa and invading the lamina propria are classified as stage Ta and T1, respectively, according to the Tumour, Node, Metastasis (TNM) classification system [52]. Intra-epithelial, high- grade (HG) tumours confined to the mucosa are classified as CIS (Tis). All of these tumours can be treated by transurethral resection of the bladder (TURB), eventually in combination with intravesical instillations and are therefore grouped under the heading of NMIBC for therapeutic purposes. The term ‘Non-muscle-invasive BC’ represents a group definition and all tumours should be characterised according to their stage, grade, and further pathological characteristics (see Sections 4.5 and 4.7 and the International Collaboration on Cancer Reporting website: http://www.iccr-cancer.org/datasets/published-datasets/urinary-male-genital/bladder. The term ‘superficial BC’ should no longer be used as it is incorrect.
4.2. Tumour, Node, Metastasis Classification (TNM)
The latest TNM classification approved by the Union International Contre le Cancer (UICC) (8th Edn.) is referred to (Table 4.1) [52].
Table 4.1: 2017 TNM classification of urinary bladder cancer
| 2017 TNM classification of urinary bladder cancer | |
| T - Primary tumour | |
| TX | Primary tumour cannot be assessed |
| T0 | No evidence of primary tumour |
| Ta | Non-invasive papillary carcinoma |
| Tis | Carcinoma in situ: ‘flat tumour’ |
| T1 | Tumour invades subepithelial connective tissue |
| T2 | Tumour invades muscle |
| T2a Tumour invades superficial muscle (inner half) | |
| T2b Tumour invades deep muscle (outer half) | |
| T3 | Tumour invades perivesical tissue |
| T3a Microscopically | |
| T3b Macroscopically (extravesical mass) | |
| T4 | Tumour invades any of the following: prostate stroma, seminal vesicles, uterus, vagina pelvic wall, abdominal wall |
| T4a Tumour invades prostate stroma, seminal vesicles, uterus or vagina | |
| T4b Tumour invades pelvic wall or abdominal wall | |
| N – Regional lymph nodes | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single lymph node in the true pelvis (hypogastric, obturator, external iliac, or presacral) |
| N2 | Metastasis in multiple regional lymph nodes in the true pelvis (hypogastric, obturator, external iliac, or presacral) |
| N3 | Metastasis in common iliac lymph node(s) |
| M - Distant metastasis | |
| M0 | No distant metastasis |
| M1a Non-regional lymph nodes | |
| M1b Other distant metastases | |
4.3. T1 subclassification
The depth and extent of invasion into the lamina propria (T1 sub-staging) has been demonstrated to be of prognostic value in retrospective cohort studies [52,53]. Its use is recommended by the most recent 2022 World Health Organization (WHO) classification [54,55]. T1 sub-staging methods are based either on micrometric (T1e and T1m) or histo-anatomic (T1a and T1b) principles; however, the optimal classification system remains to be defined [56,57].
4.4. Lymphovascular invasion
The presence of lymphovascular invasion (LVI) in TURB specimens is associated with an increased risk of pathological upstaging and worse prognosis [58-62]. Immunohistochemistry for confirmation is not mandatory [54] .
4.5. Histological grading of non-muscle-invasive bladder urothelial carcinomas
4.5.1. Types of histological grading systems
In 2004 the WHO published a histological classification system for UCs including papillary urothelial neoplasm of low malignant potential (PUNLMP), non-invasive papillary carcinoma low grade (LG) and HG. This system was also taken into the updated 2016/2022 WHO classifications [54,55]. It provides a different patient stratification between individual categories compared to the older 1973 WHO classification, which distinguished between grade 1 (G1), grade 2 (G2) and grade 3 (G3) categories [56,63].
There is a significant shift of patients between the categories of the WHO 1973 and the WHO 2004/2022 systems (see Figure 4.1), for example an increase in the number of HG patients (WHO 2004/2022) due to inclusion of a subset of G2 patients with a more favourable prognosis compared to the G3 category (WHO 1973) [64,65]. According to a multi-institutional individual patient data analysis, the proportion of tumours classified as PUNLMP (WHO 2004/2016) has decreased to very low levels in the last decade [66].
4.5.2. Prognostic value of histological grading
A systematic review and meta-analysis did not show that the 2004/2016 classification outperforms the 1973 classification in prediction of recurrence and progression [64].
To compare the prognostic value of both WHO classifications, an individual patient data analysis of 5,145 primary TaT1 NMIBC patients from 16 centres throughout Europe and one in Canada was conducted. Patients had a transurethral resection of bladder tumour (TURBT) followed by intravesical instillations at the physician’s discretion. In this large study, the WHO 1973 and the WHO 2004/2016 were both prognostic for progression but not for recurrence. When compared, the WHO 1973 was a stronger prognosticator of progression in TaT1 NMIBC than the WHO 2004/2016. However, a 3-tier (LG/G1-G2, HG/G2 & HG/G3) or a 4-tier hybrid combination LG/G1, LG/G2, HG/G2 and HG/G3) of both classification systems proved to be superior to either classification system alone, as it divides the large group of G2 patients into two subgroups (LG/HG) with different prognoses [67]. In a subgroup of 3,311 patients with primary Ta bladder tumours, a similar prognosis was found for PUNLMP and Ta LG carcinomas [66].
4.5.3. Clinical application of histological grading systems
- The WHO 2004/2022 classification system is currently supported by the WHO for clinical application. Nevertheless, the WHO 1973 is still being used.
- The most important parameters, which must be considered for clinical application of any grading system are its inter-observer reproducibility and prognostic value (see Sections 4.5.1 and 4.6).
- These guidelines provide recommendations for tumours classified by both classification systems.
Figure 4.1: Schematic representation of tumours according to grade in the WHO 1973 and 2004/2022 classifications *[67] 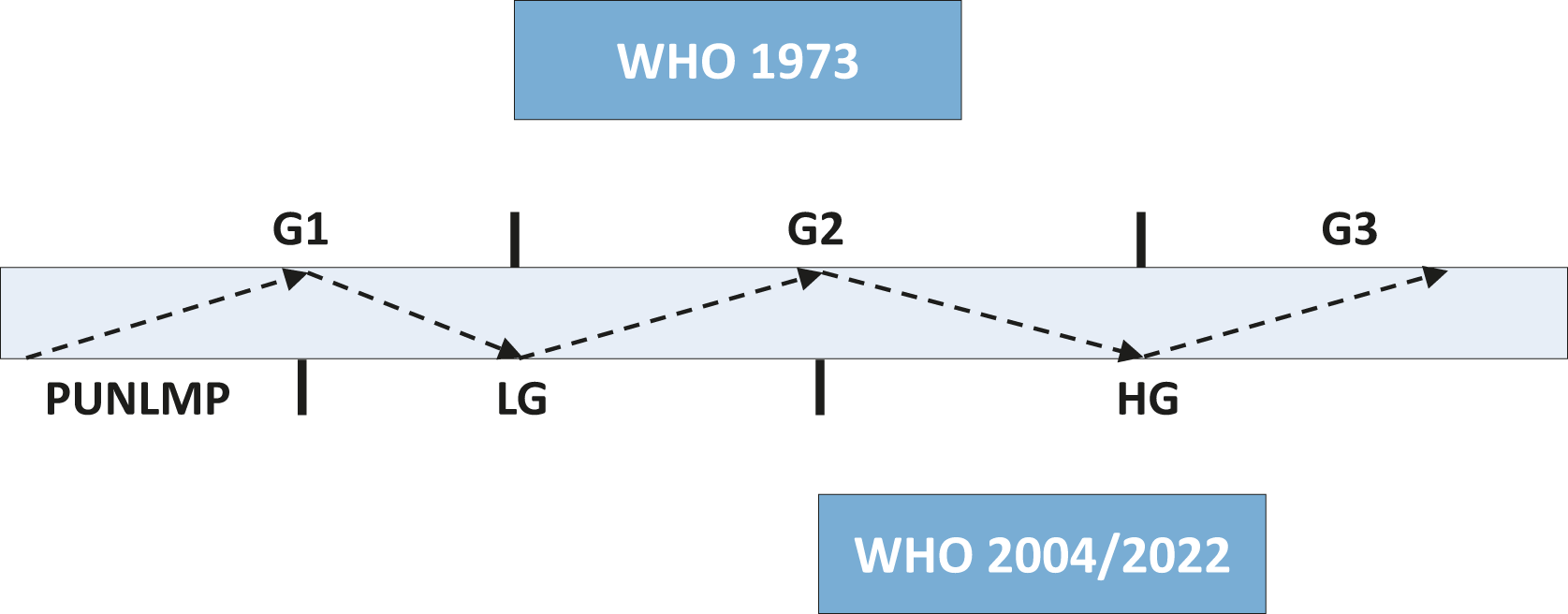 *Grade shifts from the WHO 1973 (G1–G3) to the WHO 2004/2022 (PUNLMP, LG and HG) classification for Ta/T1 bladder tumours are displayed with dotted lines and arrows. Along the dotted lines, both the degree of anaplasia and the 5-year progression rates increased in LG/G1, LG/G2, HG/G2, and HG/G3 patients. Note: the 2004/2022 WHO classification is the updated version of 2004/2016 WHO classification. According to a series of 5,145 primary Ta-T1 patients, the distribution of G1, G2 and G3 in the WHO 1973 classification is 23.5, 49.3 and 27.2%, respectively while the corresponding PUNLMP, LG and HG rates for the WHO 2004/2022 system are 1.5, 49.8 and 48.7%, respectively [67]. Figure reproduced with permission from Elsevier from [67]
*Grade shifts from the WHO 1973 (G1–G3) to the WHO 2004/2022 (PUNLMP, LG and HG) classification for Ta/T1 bladder tumours are displayed with dotted lines and arrows. Along the dotted lines, both the degree of anaplasia and the 5-year progression rates increased in LG/G1, LG/G2, HG/G2, and HG/G3 patients. Note: the 2004/2022 WHO classification is the updated version of 2004/2016 WHO classification. According to a series of 5,145 primary Ta-T1 patients, the distribution of G1, G2 and G3 in the WHO 1973 classification is 23.5, 49.3 and 27.2%, respectively while the corresponding PUNLMP, LG and HG rates for the WHO 2004/2022 system are 1.5, 49.8 and 48.7%, respectively [67]. Figure reproduced with permission from Elsevier from [67]
4.6. Carcinoma in situ
Carcinoma in situ is an intra-epithelial, HG, non-invasive UC. It can be missed or misinterpreted as an inflammatory lesion during cystoscopy if not biopsied. Carcinoma in situ is often multifocal and can occur in the bladder, but also in the upper urinary tract (UUT), prostatic ducts and urethra [68].
From a clinical point of view, CIS may be classified as [69]:
- Primary: isolated CIS with no previous or concurrent papillary tumours and no previous CIS;
- Secondary: CIS detected during follow-up of patients with a previous tumour that was not CIS;
- Concurrent: CIS in the presence of any other urothelial tumour in the bladder.
4.7. Inter- and intra-observer variability in staging and grading
There is significant variability among pathologists for the diagnosis of CIS, for which agreement is achieved in only 70–78% of cases [70]. There is also inter-observer variability in the classification of stage T1 vs. Ta tumours and tumour grading in both the 1973 and 2022 classifications. The general conformity between pathologists in staging and grading is 50–60% [71-74]. The WHO 2004/2022 classification provides slightly better reproducibility than the 1973 classification [64].
4.8. Subtypes of urothelial carcinoma
Currently the following differentiations of UC are used [75,76]:
1. Pure UC (more than 90% of all cases);
2. UC with partial (squamous-glandular or trophoblastic) divergent differentiation;
3. UC with micropapillary divergent differentiation;
4. UC with nested/microcystic divergent differentiation;
5. UC with microtubular divergent differentiation;
6. UC with large nested divergent differentiation;
7. UC with plasmacytoid divergent differentiation;
8. UC with lymphoepithelioma-like divergent differentiation;
9. UC with giant cell, diffuse, undifferentiated divergent differentiation;
10. UC with sarcomatoid divergent differentiation;
11. some UCs with other rare differentiations;
12. UCs with partial NE (neuroendocrine differentiation, % to be given);
13. pure neuroendocrine carcinoma (including small and large cell neuroendocrine carcinomas.
In the new WHO 2022 all subtypes are considered HG [55]. Up to 14.6% of NMIBC may harbour a urothelial subtype [77]. The percentage of subtype in the specimen should be reported since it has been shown to be of prognostic value [78]. The WHO 2022 classification considers all subtypes UC (LG and HG) with more than 5% of HG as a HG tumour [2,78-85]. Clinical implications of urothelial subtypes are discussed in Section 6.3.
4.9. Tumour markers and molecular classification
Tumour markers and their prognostic role have been investigated [86-90]. These methods, in particular complex approaches such as the stratification of patients based on molecular classification, are promising but have not yet been recommended by any pathological organisation and are therefore not suitable for routine application [57,91,92].
4.10. Summary of evidence and recommendations for bladder cancer classification
| Summary of evidence | LE |
| The depth of invasion (staging) is classified according to the TNM classification. | 2a |
| Tumours confined to the mucosa and invading the lamina propria are classified as stage Ta and T1, respectively. Flat, high-grade tumours that are confined to the mucosa are classified as CIS (Tis). | 2a |
| Histological grading of urothelial NMIBC is classified according to the WHO 2004/2016/2022 (PUNLMP, LG/HG) systems and/or WHO 1973 (G1–G3). | 2a |
| The WHO 2004/2016/2022 classification provides slightly better reproducibility than the 1973 classification. | 2a |
| Both the WHO 1973 and the 2004/2016/2022 classification systems are prognostic for progression, but not for recurrence. | 2a |
| The WHO 1973 is a stronger prognosticator of progression in TaT1 NMIBC than the WHO 2004/2016. However, a 3-tier hybrid (LG/G1-G2, HG/G2 & HG/G3) or a 4-tier hybrid LG/G1, LG/G2, HG/G2 and HG/G3) combination of both classification systems proved to be superior to either classification system alone. | 2a |
| Recommendations | Strength rating |
| Use the 2017 Tumour, Node, Metastasis Classification (TNM) system for classification of the depth of tumour invasion (staging). | Strong |
| Provide T1 sub-stage if the lamina propria is adequately sampled using either micrometric (T1e and T1m) or histo-anatomic (T1a and T1b) principles. | Weak |
| Use both the 1973 and 2004/2022 WHO grading classification systems, or a hybrid system. | Weak |
| Do not use the term ‘superficial’ bladder cancer. | Strong |