4. UROGENITAL TRAUMA GUIDELINES
4.1. Renal Trauma
4.1.1. Epidemiology, aetiology and pathophysiology
Renal trauma is present in up to 5% of all trauma cases [30]. It is most common in young males and has an overall population incidence of 4.9 per 100,000 [31]. Most injuries can be managed non-operatively with successful organ preservation [32,33].
Blunt injuries result from high-speed road traffic accidents/injury, falls, sporting injuries, and assault [34]. The kidney and/or hilar structures are directly crushed as a result. Less commonly, sudden deceleration may result in an avulsion injury affecting the vascular structures of the hilum or the ureteropelvic junction (UPJ).
Penetrating injuries are due to stab and gunshot wounds. They tend to be more severe and less predictable than blunt trauma. The prevalence is higher in urban settings [35]. Penetrating injury produces direct tissue disruption of the parenchyma, vascular pedicles, or collecting system. High-velocity bullets or fragments have the potential for greatest parenchymal destruction and are most often associated with multiple-organ injuries [36].
The most used classification system is that of the AAST [13]. High grade renal trauma is defined as Grade 4 and 5 injuries [37]. It is validated and predicts morbidity and the need for intervention [38,39]. This remains the most useful of urological trauma classifications although it does not differentiate between the mechanism of trauma (blunt vs. penetrating) [40]. The mechanism of trauma should be considered when applying the following guidelines with respect to the AAST classification.
Table 4.1.1: Extract of the AAST renal injury grading scale [14, 41]
| Grade* | Type of injury | Description of injury |
| 1 | Haematoma and/or Contusion | Subcapsular non-expanding haematoma or parenchymal contusion without parenchymal laceration. |
| 2 | Haematoma Laceration | Non-expanding perirenal haematoma confined to Gerota fascia. Renal parenchymal laceration < 1 cm depth without urinary extravasation. |
| 3 | Laceration | Renal parenchymal laceration > 1 cm depth without collecting system rupture or urinary extravasation. Any injury in the presence of a kidney vascular injury or active bleeding contained within Gerota fascia. |
| 4 | Laceration | Parenchymal laceration extending into urinary collecting system with urinary extravasation. Renal pelvis laceration and/or complete ureteropelvic disruption. |
| Vascular | Segmental renal vein or artery injury. Active bleeding beyond Gerota fascia into the retroperitoneum or peritoneum. Segmental or complete kidney infarction(s) due to vessel thrombosis without active bleeding. | |
| 5 | Laceration | Shattered kidney with loss of identifiable parenchymal renal anatomy. |
| Vascular | Main renal artery or vein laceration or avulsion of renal hilum. Devascularised kidney with active bleeding. |
*Advance one grade for bilateral injuries up to Grade 3.
Note: The radiology imaging criteria of the AAST renal injury scale was updated in 2018 and is presented in Table 4.1.1; some of the references in this text are still based on the AAST 1989 renal injury scale. The 2018 injury scale does not outperform the previous grading system in predicting bleeding and the need for treatment intervention and does not impact on the validity of the current recommendations [41]
4.1.2. Evaluation
The evaluation of stable patients with suspected renal trauma is now based on a trauma protocol computed tomography (CT) scan, often performed prior to involvement of a urologist [42,43]. It is important to consider all parameters in the evaluation of the patient and to understand the indications for scanning when these are not absolute. Indicators of injury include a direct blow to the flank or rapid deceleration event (fall, high-speed road traffic accidents/injury). Special consideration should be given to pre-existing renal disease [44] or the injured solitary kidney [45]. Pre-existing abnormality e.g. hydronephrosis makes injury more likely following trauma [46].
Vital signs should be recorded throughout the initial evaluation and give the most reliable indication of the urgency of the situation. Physical examination may reveal flank bruising, stab wounds, or bullet entry or exit wounds and abdominal tenderness.
Urinalysis, haematocrit and baseline creatinine are required. Haematuria (visible or non-visible) is the key finding. However, major injury such as disruption of the UPJ, pedicle injuries, segmental arterial thrombosis and stab wounds may not have haematuria [47,48]. Haematuria that is out of proportion to the history of trauma may suggest pre-existing pathology [49]. Urine dipstick quickly evaluates for haematuria, but false-negative results can range from 3-10% [50]. An increased creatinine level usually reflects pre-existing renal pathology.
4.1.3. Imaging: criteria for radiographic assessment
The goals of imaging are to grade the renal injury, document pre-existing renal pathology, demonstrate presence of the contralateral kidney and identify injuries to other organs. Haemodynamic status will determine the initial imaging pathway with unstable patients potentially requiring immediate intervention. Nearly all patients with moderate to major trauma will have had a CT scan performed soon after presentation. In patients who have not had any imaging the indications for renal imaging are [34,51-54]:
- visible haematuria;
- non-visible haematuria and one episode of hypotension;
- a history of rapid deceleration injury and/or significant associated injuries;
- penetrating trauma;
- clinical signs suggesting renal trauma e.g. flank pain, abrasions, fractured ribs, abdominal distension and/or a mass and tenderness.
4.1.3.1. Computed tomography
Computed tomography is the imaging modality of choice in stable patients. It is quick, widely available, and can accurately identify grade of renal injury [55], establish the presence of the contralateral kidney and demonstrate concurrent injuries to other organs. It is ideally performed as a three-phase study [56]:
- The arterial phase assesses vascular injury and presence of active extravasation of contrast.
- The nephrographic phase optimally demonstrates parenchymal contusions and lacerations.
- The delayed phase imaging (five minutes) identifies collecting system/ureteric injury (hypovolaemia in the trauma patient, typically means that the delayed phase performed at five minutes is unreliable for documenting collecting system/ureteric injury).
In practice, trauma patients usually undergo standardised whole-body imaging protocols and delayed phase imaging of the renal tract is not routinely performed. If there is suspicion that renal injuries have not been fully evaluated, delayed phase imaging is recommended and can be done as a repeat imaging see section (4.1.4.1.5). The rates of contrast-induced nephropathy seen in trauma patients is low [57].
4.1.3.2. Ultrasonography (US)
In the primary survey of a critically injured patient, FAST (Focused Assessment Sonography in Trauma) is used to identify hemoperitoneum as the cause of haemorrhage and hypovolemia. However, it is not routinely used for the assessment of solid organ injury as it is insensitive, operator dependant, does not define the injury well, and is inferior to CT. It is an option for follow-up [58-60].
4.1.3.3. Other imaging modalities
4.1.3.3.1. Intravenous pyelography (IVP)
Intravenous pyelography, radionuclide scans and magnetic resonance imaging (MRI) do not have a significant role in the trauma setting. The quality of one shot IVP is generally poor. Palpation of the contralateral (unaffected) kidney is a pragmatic surrogate of function [20].
The diagnostic accuracy of MRI in renal trauma is similar to that of CT [61,62]. However, the logistical challenges of MRI make this modality impractical in acute trauma.
4.1.4. Management
The management for renal trauma can be defined as non-operative (conservative or selective angioembolisation (SAE)) and operative. The majority of Grade 1-4 injuries, however, are now managed conservatively and debate has centred around updating the classification of high-grade injury i.e. identifying the injuries most likely to benefit from early selective angiographic embolisation, renal repair or nephrectomy [32,63]. There is some evidence to suggest that over 50% of patients with Grade 5 injuries confirmed on CT can be managed non-operatively; those patients selected based on lower transfusion requirements and less severe radiologic injury findings (haematoma size and renal parenchyma laceration size) [64]. Compared with operative management, non-operative management of high-grade renal trauma is associated with a lower mortality and lower nephrectomy rates [65].
4.1.4.1. Non-operative management
The non-operative management of renal trauma can be viewed as a “package of care”; a stepwise approach starting with conservative treatment, followed by interventional radiology and/or surgical exploration, if necessary. It should be noted that an algorithm for “package of care” will vary in different centres according to available interventions; however, the importance of escalation in treatment interventions should be emphasised [32]. This approach has resulted in the rate of nephrectomy for high-grade renal injuries, decreasing over time [66].
4.1.4.1.1. Blunt renal injuries
Haemodynamic stability is the primary criterion for the management of all renal injuries. Non-operative management has become the treatment of choice for most cases. In stable patients, this means a period of bed rest, serial blood tests, regular observation and re-imaging as indicated [29]. Primary conservative management is associated with a lower rate of nephrectomies, and no increase in immediate or long-term morbidity [67].
Grade 1-3 injuries are managed non-operatively [68,69]. Grade 4 injuries are also mostly treated conservatively, but the requirement for subsequent intervention is higher [70]. Persistent urinary extravasation from an otherwise viable kidney after blunt trauma usually responds to ureteric stent placement and/or percutaneous drainage [71].
Grade 5 injuries often present with haemodynamic instability and major associated injuries. There is thus a higher rate of exploration and nephrectomy [72,73]. However, several studies now support expectant management in patients with Grade 4 and 5 injuries [32,33,74-78]. Similarly, unilateral main arterial injuries or arterial thrombosis are normally managed non-operatively in haemodynamically stable patients with surgical repair reserved for bilateral artery injuries or injuries involving a solitary functional kidney [79]. Pre-hospital prolonged warm ischaemia usually results in irreparable damage and renal loss.
One study designed a nomogram to predict the need for an intervention to stop bleeding in high-grade renal trauma. Factors which increased risk of intervention were a haematoma size of > 12 cm, penetrating trauma, vascular contrast extravasation, pararenal haematoma extension, concomitant injuries, and shock [80].
4.1.4.1.2. Penetrating renal injuries
Penetrating abdominal wounds have traditionally been managed surgically. However, selective non-operative management of penetrating abdominal wounds is now accepted following detailed assessment in stable patients [70,81-83].
For renal injuries, the site of the wound, haemodynamic stability, and diagnostic imaging are the main determinants for intervention. The majority of low-grade stab wounds posterior to the anterior axillary line can be managed non-operatively in stable patients [84]. Grade 3 or higher injuries due to stab wounds in stable patients can be managed expectantly but warrant closer observation as the clinical course is more unpredictable and associated with a higher rate of delayed intervention [84,85]. High-grade injuries, concomitant abdominal injuries and gunshot wounds are most likely to fail non-operative management [83]. A gunshot wound is an independent risk factor for nephrectomy in grade 4 and 5 traumatic renal injuries, compared with stab wounds [86]. Overall, non-operative management of penetrating injuries in selected stable patients is associated with a successful outcome in up to 50% of stab wounds and up to 40% of gunshot wounds [33,87-90].
4.1.4.1.3. Selective angioembolisation
Selective angioembolisation has a key role in the non-operative management of blunt renal trauma in haemodynamically stable patients [91]. Currently there are no validated criteria to identify patients who require SAE and its use in renal trauma remains variable. Accepted CT findings indicating the need for SAE are active extravasation of contrast, arteriovenous fistula (AVF) and pseudo-aneurysm [92]. The presence of both active contrast extravasation and a large perirenal haematoma (> 25 mm depth) predict, with good accuracy, the need for SAE [92,93].
Selective angioembolisation has been utilised in the non-operative management of all grades of renal injury; however, it is likely to be most beneficial in the setting of high-grade renal trauma (AAST > 3) [94-96]. Non-operative management of high-grade renal trauma, where SAE is included in the management algorithm, can be successful in up to 94.9% of Grade 3, 89% of Grade 4 and 76% of Grade 5 injuries [91,94,97-99]. Increasing grade of renal injury is associated with increased risk of failed SAE and need for repeat intervention [100]. Although success rates of SAE are relatively high, gross haematuria, haemodynamic instability, Grade 5 trauma and urinary extravasation are independent predictors of SAE failure in patients of all ages who undergo upfront SAE for moderate to high-grade non-iatrogenic blunt renal trauma [97]. SAE, when compared with surgical repair, is associated with a reduced rate of subsequent nephrectomy in the management of blunt and penetrating high-grade renal trauma (Grade 4 and Grade 5) [101].
Repeat embolisation prevents nephrectomy in 67% of patients. Open surgery after failed embolisation usually results in nephrectomy [100,102]. Despite concerns regarding parenchymal infarction and the use of iodinated contrast media, SAE does not appear to affect the occurrence or outcome of acute kidney injury following renal trauma [103]. For high-grade injuries, SAE has also been shown to have a high success rate and to provide the greatest protection of renal function, with no difference in renal function after long-term follow-up [104]. In severe polytrauma or high operative risk, the main artery may be embolised, either as a definitive treatment or as a step to a more controlled nephrectomy.
The evidence supporting SAE in penetrating renal trauma is sparse as penetrating injuries are much less common than blunt. One study found that AE is three times more likely to fail in penetrating trauma [81]. However, SAE has been used successfully to treat acute haemorrhage, AVF and pseudo-aneurysms resulting from penetrating renal trauma [105].
4.1.4.1.4. Ureteral stenting and urinary catheterisation
In the management of high-grade renal trauma with collecting system injuries, ureteral stenting in asymptomatic patients has proven no clear benefits. Current evidence suggests intervention (ureteral stenting, nephrostomy or perirenal drainage) only when patients develop symptoms (flank pain, fever, leucocytosis) related to persistent urinary leaks [71,106].
Urethral catheterisation is not necessary in stable patients with low-grade injury. Patients with severe visible haematuria, who require monitoring or ureteric stenting, benefit from catheterisation. A longer period of catheterisation is required if a ureteric stent is placed. Once the haematuria lightens and the patient is mobile, the catheter should be removed.
4.1.4.1.5. Repeat imaging (early)
Computed tomography scans should be performed on patients with fever, unexplained decreased haematocrit, or significant flank pain. Repeat imaging is also recommended in high-grade injury and in penetrating trauma two to four days after trauma to minimise the risk of missed complications. Repeat imaging can be safely omitted for patients with Grade 1-3 injuries if they remain clinically well [107-110].
4.1.4.2. Surgical management
4.1.4.2.1. Indications for renal exploration
A non- or transient- response to initial fluid resuscitation is a strong indication for exploration [81,82]. There is a trend towards ongoing resuscitation and AE [111] but inadequate response to intravenous fluid resuscitation and a blood lactate ≥ 4 mmol/L are predictive factors for nephrectomy [112]. Exploration is influenced by aetiology and grade of injury, transfusion requirements, the need to explore associated abdominal injuries, and the discovery of an expanding or pulsatile peri-renal haematoma at laparotomy [113]. Haemodynamic unstable grade 5 vascular injuries are an indication for exploration [97,114].
4.1.4.2.2. Operative findings and reconstruction
The overall exploration rate for blunt trauma is low [115]. The goals of exploration following renal trauma are vascular control and renal salvage. Most series recommend the transperitoneal approach for surgery [116,117]. Exposing the retroperitoneum and leaving the confined haematoma undisturbed for as long as possible is recommended but not always practically achievable; temporarily packing the fossa tightly with laparotomy gauze swabs may be required to help minimise haemorrhage. Broad exposure of the retroperitoneum to manage inframesocolic zone I and zone II trauma can be achieved through a right medial visceral rotation (Cattell-Braasch Manoeuvre) and allows quick access to the great vessels and renal vasculature for clamping to achieve urgent haemorrhage control if required. The principal surgical steps of the Cattell-Braasch manoeuvre are to mobilise the caecum and ascending colon by incising along the white line of Toldt and then incising along the plane between the root of the small bowel mesentery and posterior peritoneum, in order to ‘lift’ the colon and small bowel up on the chest [118,119]
Stable haematomas detected during exploration for associated injuries should not be opened. Central or expanding haematomas indicate injuries of the renal pedicle, aorta, or vena cava and are potentially life-threatening and warrant further exploration [120]. Further dissection and isolation of the individual renal vessels may then be required as part of the assessment towards renal salvage [121].
Feasibility of renal reconstruction should be judged during the operation [109]. The overall rate of patients who undergo a nephrectomy during exploration is approximately 30% but can be as high as 85% when opening zone II Gerota’s phasia [122,123]. Other intra-abdominal injuries also increase the likelihood of nephrectomy [124]. Mortality is associated with overall severity of the injury and not often a consequence of the renal injury itself [125]. High velocity gunshot injuries make reconstruction difficult, and nephrectomy is usually required [126].
Renorrhaphy is the most common reconstructive technique. Partial nephrectomy is required when non-viable tissue is detected. Watertight closure of the collecting system is desirable, although closing the parenchyma over the injured collecting system is acceptable.
The use of haemostatic agents and sealants in reconstruction is helpful [127]. In all cases, drainage of the ipsilateral retroperitoneum is recommended.
The repair of vascular injuries is seldom, if ever, effective [128]. Repair should be attempted in patients with a solitary kidney or bilateral injuries [129]. Nephrectomy for main renal artery injury has outcomes similar to those of vascular repair and does not worsen post-treatment renal function in the short-term. Bleeding or dissection of the main renal artery may also be managed with a stent.
4.1.5. Follow-up
The risk of complications relates to aetiology, injury grade, and mode of management [130,131]. Follow-up includes physical examination, urinalysis, diagnostic imaging, blood pressure measurement and serum creatinine [72]. Potential complications are primarily identified by imaging; however, follow-up imaging is not recommended in low-grade uncomplicated injury. Ultrasound can be used to define the post-injury anatomy avoiding further ionising radiation. Nuclear medicine scans may be useful for documenting baseline functional recovery following renal trauma injury and reconstruction [132]. Annual blood pressure monitoring is recommended to exclude renovascular hypertension [133].
4.1.5.1. Complications
Early (≤ 1 month) complications include bleeding, infection, perinephric abscess, sepsis, urinary fistula, hypertension, urinary extravasation, and urinoma. Delayed complications include bleeding, calculus formation, chronic pyelonephritis, hypertension, AVF, hydronephrosis and pseudo-aneurysms. Bleeding may be life-threatening with elective angiographic embolisation the preferred treatment [134]. Perinephric abscess formation is initially managed by percutaneous drainage [115].
Hypertension is rare [135,136]. It may occur acutely because of external compression from peri-renal haematoma (Page kidney), chronically due to compressive scar formation, or resulting from renal artery thrombosis, segmental arterial thrombosis, renal artery stenosis (Goldblatt kidney), or AVF. Arteriography may be required. Treatment, including medical management, excision of the ischaemic parenchymal segment, vascular reconstruction, or nephrectomy, is indicated if hypertension persists [133].
Arteriovenous fistulae usually present with delayed onset of significant haematuria, most often after penetrating trauma. Percutaneous embolisation is often effective for symptomatic AVF, but larger fistulae may require surgery [137]. The development of pseudo-aneurysm is a rare complication following blunt trauma.
4.1.6. Iatrogenic renal injuries
Iatrogenic renal trauma needs to be recognised and managed promptly to minimise morbidity and mortality. The most common causes of iatrogenic renal injuries are percutaneous access to kidney, stone surgery, cancer surgery (laparoscopic and open) and transplantation [3]. The diagnosis and management follow the same principles as outlined in Section 4.1.4. above.
4.1.7. Summary of evidence and recommendations for evaluation and management of renal trauma
| Summary of evidence | LE |
| Vital signs on admission give the most reliable indication of the urgency of the situation. | 3 |
| Special consideration should be given to patients with a solitary kidney and pre-existing renal disease. | 4 |
| Haematuria is a key finding following renal trauma; although, it may not be present in certain situations. | 3 |
| A multi-phase CT scan is the best method for the diagnosis and staging of renal injuries in haemodynamically stable patients. | 3 |
| Haemodynamic stability is the primary criterion for selecting patients for non-operative management. | 3 |
| Ureteric stenting in stable asymptomatic Grade 4 renal injuries is not necessary. | 3 |
| Selective angioembolisation is effective in patients with active bleeding from renal injury, without other indications for immediate abdominal operation. | 3 |
| Renal reconstruction should be attempted if haemorrhage is controlled and there is sufficient viable renal parenchyma. | 3 |
| Iatrogenic renal injuries are procedure-dependent (1.8-15%); the most common injuries are vascular. | 3 |
| Limited literature exists with regard to long-term consequences of renal trauma. Current follow-up includes physical examination, urinalysis, diagnostic imaging, serum creatinine, as well as annual blood pressure monitoring to diagnose renovascular hypertension. | 4 |
| Recommendations | Strength rating |
| Evaluation | |
| Assess haemodynamic stability upon admission. | Strong |
| Record past renal surgery, and known pre-existing renal abnormalities (ureteropelvic junction obstruction, solitary kidney, urolithiasis). | Strong |
| Test for haematuria in a patient with suspected renal injury. | Strong |
Perform a multi-phase computed tomography (CT) scan in trauma patients with:
| Strong |
| Management | |
| Manage stable patients with blunt renal trauma non-operatively with close monitoring and re-imaging as required. | Strong |
| Manage isolated Grade 1-4 stab and low-velocity gunshot wounds in stable patients non-operatively. | Strong |
| Use selective angioembolisation for active renal bleeding if there are no other indications for immediate surgical exploration. | Strong |
| Insert urinary system drainage (ureteral stenting, nephrostomy) or perirenal drainage in cases of persistent or symptomatic urinary leak. | Strong |
| Proceed with renal exploration in the presence of persistent haemodynamic instability due to renal injury after failure of non-operative management. | Strong |
| Perform renal exploration in case of expanding or pulsatile peri-renal haematoma during laparotomy for associated injuries. | Strong |
| Attempt renal reconstruction if haemorrhage is controlled and there is sufficient viable renal parenchyma. | Weak |
| Repeat imaging in high-grade and penetrating injuries and in cases of fever, worsening flank pain, or falling haematocrit. | Strong |
| Follow-up approximately three months after major renal injury with urinalysis, individualised radiological investigation, e.g., nuclear scintigraphy, CT or ultrasound, blood pressure measurement and renal function tests. Longer term annual follow-up for blood pressure is recommended. | Weak |
4.1.8. Treatment algorithms
Management of renal trauma
Figure 4.1.1 Management of renal trauma 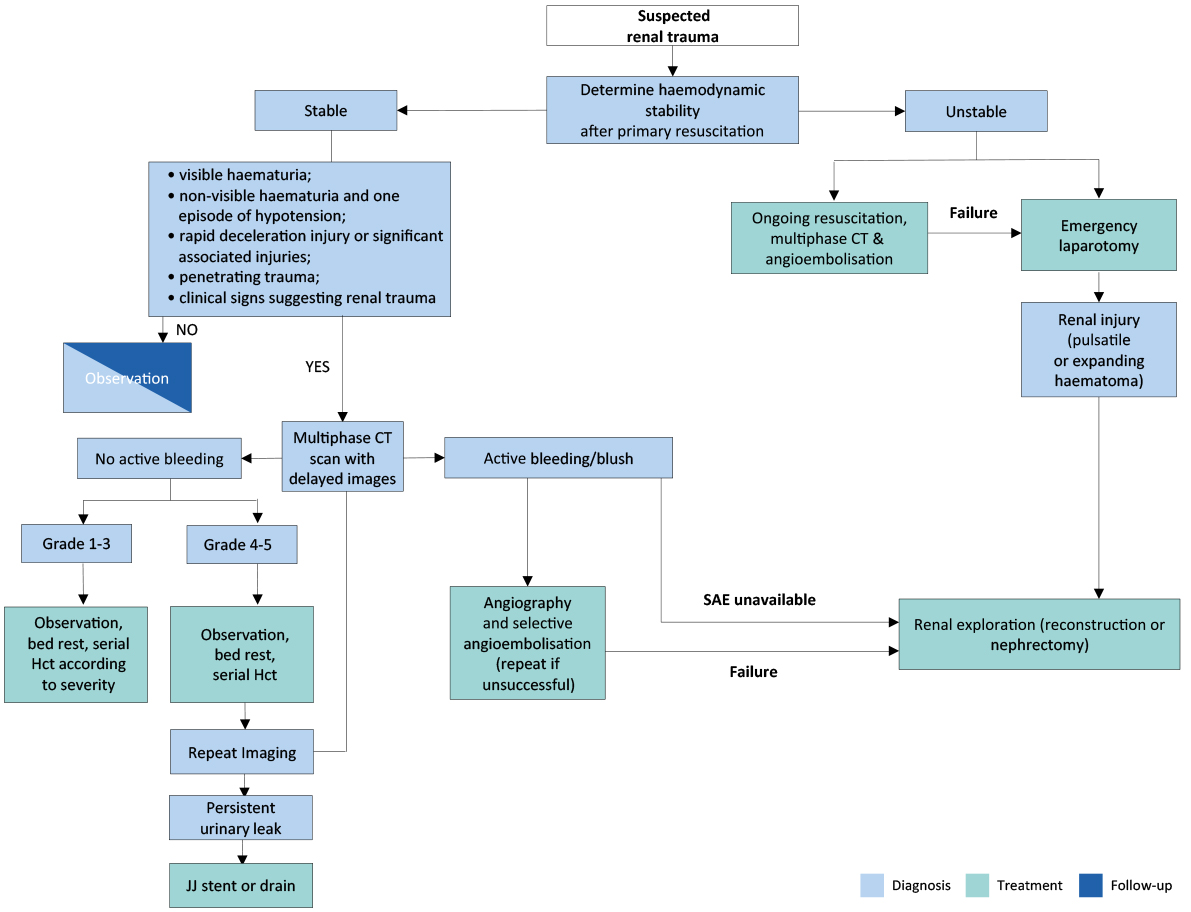 --- If haemodynamically unstable.
--- If haemodynamically unstable.
CT = computed tomography; Ht = haematocrit; SAE = selective angioembolisation.
4.2. Ureteral Trauma
4.2.1. Incidence
Trauma to the ureters is relatively rare as they are protected by their small size, mobility, posterior location, and the adjacent musculoskeletal and visceral structures. Iatrogenic injury during open, laparoscopic and endoscopic surgery is responsible for the majority of cases [138]. The injury is often missed intra-operatively and may result in significant morbidity [139].
4.2.2. Epidemiology, aetiology, and pathophysiology
Overall, ureteral trauma accounts for 1-2.5% of urinary tract trauma [138,140-142], Penetrating external ureteral trauma, mostly by gunshot wounds, is the commonest form in most modern series, [138,140,143]. Higher rates of ureteral injury are seen in modern combat injuries [127]. About one-third of cases of external trauma to the ureters are caused by blunt trauma, mostly road traffic accidents [141,142].
Ureteral injury should be suspected in all cases of penetrating abdominal injury, although it occurs in just 2-3% of cases [138]. It should also be suspected in blunt trauma with significant deceleration as pelvi-ureteral disruption can result [138]. The distribution of external ureteral injuries along the ureter varies between series, but it is commonest in the upper ureter [140-142].
The incidence of urological iatrogenic trauma has decreased in the last twenty years due to improvements in technique, instrument technology, training methods and subspecialisation [143,144].
Iatrogenic ureteral trauma can result from:
- ligation with a suture, crushing by a surgical instrument;
- partial or complete transection by unintended scalpel incision;
- thermal injury;
- or ischaemia from devascularisation [143,145,146].
Injury usually involves the lower ureter [138,143,145,147]. Gynaecological operations are the most common cause of significant iatrogenic trauma. It also occurs in colorectal operations, (resection of the distal colon) and vascular surgery (aortic aneurysm repair) [148,149]. There has been a significant decrease in the rate of ureteral injury during robot-assisted procedures [150] and colorectal surgery [45]. However, minimally invasive techniques have not further reduced the rate of ureteral injuries in gynaecological surgery [151-153].
Ureteroscopy is a common cause of iatrogenic ureteric trauma contributing up to 71.6% in some series [154]. The post-ureteroscopic lesion scale (PULS) aims to standardise intra-operative traumatic findings during ureteroscopy [155]. Predictors for high grade ureteric injury include male gender, longer operative times, and ureteral access sheath (UAS) insertion times [154].
A smaller proximal ureter diameter seen in CT scanning and a predictor for high-grade ureteral injury during UAS placement [156]. A small RCT using pre-operative silodosin 8 mg for three days significantly reduced Grade 2 or higher ureteral injuries due to UAS insertion [157].
Risk factors for iatrogenic trauma include conditions that alter the normal anatomy, e.g., advanced malignancy, prior surgery or irradiation, diverticulitis, endometriosis, anatomical abnormalities, and major haemorrhage [143,148,158,159]. Occult ureteral injury occurs more often than reported and not all injuries are diagnosed intra-operatively [139].
4.2.3. Diagnosis
The diagnosis of ureteral trauma is challenging; therefore, a high index of suspicion should be maintained. In penetrating external trauma, it is best identified intra-operatively during laparotomy [160]. The diagnosis is delayed in most cases of blunt trauma and iatrogenic trauma [143,147,161].
4.2.3.1. Clinical diagnosis
External ureteral trauma usually accompanies severe abdominal and pelvic injuries. Penetrating trauma is usually associated with vascular and intestinal injuries, while blunt trauma is associated with damage to the pelvic bones and lumbosacral spinal injuries [141,142]. Haematuria is an unreliable and poor indicator of ureteral injury, as it is present in only 50-75% of patients [138,143,162].
Iatrogenic injury may be noticed during the primary procedure, when intravenous dye (e.g. indigo carmine) is injected to exclude ureteral injury. Early recognition facilitates immediate repair and provides a better outcome [158,160]. However, it is usually presenting later in the same admission, with the untoward sequelae of ureteral injury-upper tract obstruction, sepsis, abdominal distension, and when it is discovered by subsequent evidence of upper tract obstruction, urinary fistulae formation or sepsis. The following clinical signs are characteristic of delayed diagnosis-flank pain, urinary incontinence, vaginal or drain urinary leakage, haematuria, fever, and uraemia or urinoma. The complication rate increases with delayed diagnosis [138,161,163].
4.2.3.2. Radiological diagnosis
Multi-phase CT is the mainstay imaging technique for trauma patients. Generally, it is widely available and allows for multi-phasic assessment of all of the structures in the pelvis and abdomen. Computed tomography urography (CTU) is the examination of choice when ureteral injuries are suspected [164,165]. Extravasation of contrast medium in the delayed phase is the hallmark sign of injury. However, hydronephrosis, ascites, urinoma or mild ureteral dilation are often the only signs. In unclear cases, a retrograde or antegrade urography is the best method for confirmation [143]. Intravenous pyelography, especially one-shot IVP, is unreliable in diagnosis, as it is negative in up to 60% of patients [138,143].
4.2.4. Prevention of iatrogenic trauma
The prevention of iatrogenic trauma to the ureters depends upon the visual identification of the ureters and careful intra-operative dissection in their proximity [143,145,146]. The use of prophylactic pre-operative ureteral stent insertion assists in visualisation and palpation can be used in cases of higher complexity [14,166]. According to a systematic review (SR) on the use of prophylactic/lighted stent (PUS/LUS) or infrared fluorescent ureteral catheter (NIRFUC) in colorectal surgery, there was no significant decrease in ureteral injuries when using these stents [167]. In a recent meta-analysis, a potential benefit of prophylactic stenting in gynaecological surgery was observed. However, there’s a risk of selection bias, with more high-risk patients in most of the prophylactic stenting groups [145,168,169]. A retrograde instillation of indocyanine green in the ureters has been shown to safely allow their identification and preservation in complex robotic-assisted colorectal surgeries [170,171], however has no proven preventative effect on ureteral injury [167].
An RCT studying the use of silodosin in the prevention of ureteral injury after access sheet placement in ureterorenoscopy showed beneficial results, with a significant decrease in ureteral trauma [157].
4.2.5. Management
Management of ureteral trauma depends on many factors including the aetiology, severity, and location of the injury. Immediate diagnosis of a ligation injury during an operation can be managed by de-ligation and stent placement. Partial injuries can be repaired immediately with a stent or urinary diversion via a nephrostomy tube. Stenting is helpful because it provides canalisation and may decrease the risk of stricture [143,172,173]. Stent placement can be performed, antegradely, retrogradely or combined (rendezvous technique) [174].
Immediate repair of complete ureteral injury is advisable as it significantly decreases the need for secondary or tertiary procedures compared to delayed repair [172]. The ureter is mobilised on both ends and a spatulated end-to-end anastomosis is performed. Primary repair by uretero-ureterostomy or ureteric re-implantation can be safely performed laparoscopically at the time of the iatrogenic injury, with good medium-term results [175]. In cases of unstable trauma patients, a ‘damage control’ approach is preferred with ligation of the ureter, diversion of the urine (e.g. via a nephrostomy), and a later delayed definitive repair [176].
A national trauma database study reported that the majority of blunt low- and high-severity traumatic ureteric injuries in both stable and unstable patients were treated by nephrostomy or stenting [177]. Exploratory laparotomy for associated traumatic injuries was a predictor for immediate ureteral reconstruction [177]. Injuries that are diagnosed late are usually managed first by placement of a nephrostomy tube or stent [143].
Endo-urological treatment of delayed-diagnosed ureteral injuries by internal stenting, with or without dilatation, is the first step in most cases. It is performed either retrogradely or antegradely via a percutaneous nephrostomy, and it has a variable success rate of 14-19% [178-180]. An open or robot-assisted laparoscopic surgical repair is necessary in case of failure [181]. The basic principles for any surgical repair of a ureteral injury are outlined in Table 4.2.2. Wide debridement is highly recommended for gunshot wound injuries due to the ‘blast effect’ of the injury.
4.2.5.1. Proximal and mid-ureteral injury
Injuries shorter than 2-3 cm can usually be managed by a primary uretero-ureterostomy [138]. When this approach is not feasible, a ureterocalicostomy should be considered. In case of a large extra-renal pelvis and a stricture at the UPJ, a pelvic spiral flap (Culp de Weerd) is an option [182]. In extensive ureteral loss, a transureteroureterostomy is a valid option. The proximal stump of the ureter is transposed across the midline and anastomosed to the contralateral ureter. The reported stenosis rate is 4% and re-intervention or revision occurs in 10% of cases [183].
4.2.5.2. Distal ureteral injury
Distal injuries are best managed by ureteral re-implantation (ureteroneocystostomy) because the primary trauma jeopardises the blood supply to the distal ureter. The question of refluxing vs. non-refluxing ureteral re-implantation remains unresolved in the literature. The risk for clinically significant reflux should be weighed against the risk for ureteral obstruction.
A psoas hitch between the bladder and the ipsilateral psoas tendon is usually needed to bridge the gap and to protect the anastomosis from tension. The contralateral superior vesical pedicle may be divided to improve bladder mobility. The reported success rate is very high (97%) [183]. In extensive mid-lower ureteral injury, the large gap can be bridged with a tabularised L-shaped bladder flap (Boari flap). It is a time-consuming operation and unsuited to the acute setting. The success rate is reported to be 81-88% [184].
4.2.5.3. Long segment ureteral injury
A longer ureteral injury can be replaced using a segment of the intestines, usually the ileum (ileal interposition graft). This should be avoided in patients with impaired renal function or known intestinal disease. Follow-up includes serum chemistry to diagnose hyperchloremic metabolic acidosis [185]. The long-term complications include anastomotic stricture (3%) and fistulae (6%) [186]. Another option is downward nephropexy and a long Boari flap. In cases of extensive ureteral loss or after multiple attempts at ureteral repair, the kidney can be relocated to the pelvis (auto-transplantation). The renal vessels are anastomosed to the iliac vessels and a ureteral re-implantation is performed [187,188].
Buccal mucosa ureteroplasty is an option for long segment ureteral injury, especially after a previous failed reconstruction, as an alternative to auto-transplantation. The overall success rate is 90%, but experience is limited [189].
4.2.5.4. Permanent urinary diversion/nephrectomy
Following early or late repairs, up to 38% of patients develop secondary ureteric strictures requiring interventions [190] or palliative management by indwelling ureteric catheter or nephrostomy tube [172,191]. Moreover, in some series up to 10% of failed repairs have evidence of renal parenchyma or function loss, leading to nephrectomy [172,190].
Table 4.2.2: Principles of surgical repair of ureteral injury
| Debridement of necrotic tissue |
| Spatulation of ureteral ends |
| Watertight tension-free mucosa-to-mucosa anastomosis using absorbable sutures |
| Internal stenting |
| External drain |
| Isolation of injury with peritoneum or omentum |
4.2.6. Summary of evidence and recommendations for the management of ureteral trauma
| Summary of evidence | LE |
| Iatrogenic ureteral trauma is the most common cause of ureteral injury. | 3 |
| Gunshot wounds account for the majority of penetrating ureteral injuries, while road traffic accidents account for most blunt injuries. | 3 |
| Ureteral trauma usually accompanies severe abdominal and pelvic injuries. | 3 |
| Haematuria is an unreliable and poor indicator of ureteral injury. | 3 |
| Pre-operative prophylactic stents do not prevent ureteral injury; however, they may assist in its detection. | 2 |
| Endo-urological treatment of small ureteral fistulae and strictures is safe and effective. | 3 |
| Major ureteral injury requires ureteral reconstruction following temporary urinary diversion. | 3 |
| Recommendations | Strength rating |
| Visually identify the ureters to prevent ureteral trauma during complex abdominal and pelvic surgery. | Strong |
| Beware of concomitant ureteral injury in all abdominal penetrating trauma, and in deceleration-type blunt trauma. | Strong |
| Use pre-operative prophylactic stents in high-risk of ureteral injuries. | Weak |
| Repair iatrogenic ureteral injuries recognised during surgery immediately. | Strong |
| Treat iatrogenic ureteral injuries with delayed diagnosis by nephrostomy tube/JJ stent urinary diversion. | Strong |
| Manage ureteral strictures by ureteral reconstruction according to the location and length of the affected segment. | Strong |
4.2.7. Treatment algorithms
Management of ureteral injuries
Figure 4.2.1: Management of ureteral injuries

4.3. Bladder Trauma
4.3.1. Classification
Bladder trauma is primarily classified according to the location of the injury: intraperitoneal, extraperitoneal, and combined intra-extraperitoneal [192], as it guides further management [193]. Bladder trauma is categorised by aetiology: non-iatrogenic (blunt and penetrating) and iatrogenic (external and internal).
4.3.2. Epidemiology, aetiology, and pathophysiology
Road traffic accidents are the most common cause of blunt bladder injury, followed by falls and other accidents. The main mechanisms are pelvic crush and blows to the lower abdomen [141,192,194]. Most patients with blunt bladder injury have associated pelvic fractures (60-90%) and other intra-abdominal injuries (44-68.5%) [195,196]. Pelvic fractures are associated with bladder injury in about 3% of cases [141,197]; however, this can be as high as 26.5% in cases of severe pelvic injury [198]. Bladder injury is associated with urethral injury in 5-20% of cases [193,196,199]. Alcohol intoxication is associated with increased risk of bladder injury in patients suffering from a motor vehicle collision [200].
Combined intra- and extraperitoneal ruptures are present in 5-8% of all bladder ruptures, with extraperitoneal (54-56%), and intraperitoneal (38-40%) [201]. The incidence of extraperitoneal (22.4-61.1%), and intraperitoneal (38.9-65.8%) injuries varies among series [201]. Extraperitoneal injury is almost always associated with pelvic fractures [194,196]. It is usually caused by distortion of the pelvic ring, with shearing of the anterolateral bladder wall near the bladder base (at its fascial attachments), or by a contrecoup at the opposite side. The highest risk of bladder injury was found in disruptions of the pelvic circle with displacement > 1 cm, diastasis of the pubic symphysis > 1 cm, and pubic rami fractures [141,193]. Occasionally, the bladder is directly perforated by a sharp bony fragment [193].
Intraperitoneal injury is caused by a sudden rise in intravesical pressure of a distended bladder, secondary to a blow to the pelvis or lower abdomen. The bladder dome is the weakest point of the bladder and ruptures usually occur there [193]. Penetrating injuries, mainly gunshot wounds, are rare except in conflict zones and violent urban areas [192,202,203]. Improvised explosive devices are the main cause of combat related bladder injuries in asymmetric warfare [204].
4.3.2.1. Iatrogenic bladder trauma (IBT)
The bladder is the urological organ that is most commonly affected by iatrogenic injury [205]. External IBT occurs most often during obstetric and gynaecological procedures, followed by urological and general surgical operations [205]. Main risk factors are previous surgery, inflammation and malignancy [205]. Bladder perforations occur in up to 4.9% of mid-urethral sling operations for stress urinary incontinence in women. This rate is significantly lower in the obturator route compared to the retropubic route [206].
Internal IBT mainly occurs during transurethral resection of the bladder (TURB). Reported risk factors are larger tumours, older age, pre-treated bladders (previous TURB, intravesical instillations) and location at the bladder dome [207,208]. Tumours at the lateral wall pose a risk factor because of the obturator jerk [209,210]. Extraperitoneal perforations are more frequent than intraperitoneal perforations [208,211], and perforations requiring intervention are rare (0.16-0.57%) [207].
4.3.3. Diagnostic evaluation
The principal sign of bladder injury is visible haematuria [193,194]. Absolute indications for bladder imaging include: visible haematuria and a pelvic fracture [193] or non-visible haematuria combined with high-risk pelvic fracture (disruption of the pelvic circle with displacement > 1 cm or diastasis of the pubic symphysis > 1 cm) or posterior urethral injury [193]. Bladder trauma should also be suspected in patients with blunt urethral trauma and high Injury Severity Score (ISS) [212]. In the absence of these absolute indications, further imaging is based on clinical signs and symptoms including [193,194,202,213]:
- inability to void or inadequate urine output;
- abdominal tenderness or distension due to urinary ascites, or signs of urinary ascites in abdominal imaging;
- uraemia and elevated creatinine level due to intraperitoneal re-absorption;
- entry/exit wounds at lower abdomen, perineum or buttocks in penetrating injuries.
Intra-operative signs of external iatrogenic bladder injury include: extravasation of urine, visible laceration, visible bladder catheter, and blood and/or gas in the urine bag during laparoscopy [214]. Direct inspection is the most reliable method of assessing bladder integrity [205]. Retrograde bladder filling (with or without instillation of dye e.g., methylene blue) helps to detect smaller lesions [215,216]. If bladder perforation is close to the trigone, the ureteric orifices should be inspected [205,214].
Internal bladder injury is recognised by cystoscopic identification of fatty tissue, dark space, or bowel [217]. It may also be detected by the inability to distend the bladder, low return of irrigation fluid, or abdominal distension [218].
Post-operatively, missed bladder trauma is diagnosed by haematuria, abdominal pain, abdominal distension, ileus, peritonitis, sepsis, urine leakage from the wound, decreased urinary output, or increased serum creatinine [205,214]. An IBT during hysterectomy or caesarean delivery can result in vesicovaginal or vesicouterine fistulae [214,219].
4.3.3.1. Cystography
Cystography is the preferred diagnostic modality for non-iatrogenic bladder injury and for a suspected IBT in the post-operative setting [219,220]. Both plain and CT cystography have a comparable sensitivity (90-95%) and specificity (100%) [194,221]. However, CT cystography is superior in the identification of bony fragments in the bladder and bladder neck injuries, as well as concomitant abdominal injuries [193,196].
Cystography must be performed using retrograde filling of the bladder with a minimum volume of 300-350 mL of dilute contrast material [220,222]. Passive bladder filling by clamping the urinary catheter during the excretory phase of CT or IVP is not sufficient to exclude bladder injury [194]. Intraperitoneal extravasation is visualised by free contrast medium in the abdomen outlining bowel loops or abdominal viscera [223]. Extraperitoneal bladder injury is typically diagnosed by flame-shaped areas of contrast extravasation in the peri-vesical soft tissues. Contrast medium in the vagina is a sign of vesicovaginal fistula [219].
4.3.3.2. Cystoscopy
Cystoscopy is the preferred method for detection of intra-operative bladder injuries as it may directly visualise the laceration and can localise the lesion in relation to the position of the trigone and ureteral orifices [223]. A lack of bladder distension during cystoscopy suggests a large perforation. Cystoscopy is recommended to detect perforation of the bladder (or urethra) following retropubic sub-urethral sling operations [206,224]. Routine intra-operative cystoscopy during other gynaecologic procedures is not recommended [225], although the threshold to perform it should be low in any suspected bladder injury.
4.3.4. Prevention
The risk of bladder injury is reduced by emptying the bladder by urethral catheterisation in every procedure where the bladder is at risk [215,226]. Furthermore, the catheter’s balloon can aid in identification of the bladder [215]. During TURB for tumours at the lateral wall, the incidence of internal IBT can be reduced by obturator nerve block or adequate muscle relaxation [210]. There is conflicting evidence whether bipolar TURB can reduce the risk for an obturator jerk [209,210]. The use of combat pelvic protection systems reduces the risk of bladder and other genitourinary injuries due to the blast mechanism of improvised explosive devices [204,227].
4.3.5. Disease management
4.3.5.1. Conservative management
Conservative treatment, which comprises of clinical observation and continuous bladder drainage [208], is the standard treatment for an uncomplicated extraperitoneal injury due to blunt [193,196,199] or iatrogenic trauma [208].
Conservative treatment can also be chosen for uncomplicated intraperitoneal injury after TURB or other operations, but only in the absence of peritonitis and ileus [223,228]. Placement of an intraperitoneal drain is advocated, especially when the lesion is larger [218,229]. Penetrating extraperitoneal bladder injuries (only if minor and isolated) can also be managed conservatively [213,230,231].
4.3.5.2. Surgical management
Bladder closure is performed with absorbable sutures [205,230]. There is no evidence that two-layer is superior to watertight single-layer closure [196,230].
4.3.5.2.1. Blunt non-iatrogenic trauma
Most extraperitoneal ruptures can be treated conservatively; however, bladder neck involvement, bone fragments in the bladder wall, concomitant rectal or vaginal injury or entrapment of the bladder wall necessitate surgical intervention [193,232]. There is an increasing trend to treat pelvic ring fractures with open stabilisation and internal fixation with osteosynthesis material. During this procedure, an extraperitoneal rupture should be sutured concomitantly in order to reduce the risk of infection [233]. Likewise, an extraperitoneal rupture should be sutured during surgical exploration for other injuries, in order to decrease the risk of complications and to reduce recovery time [199]. In case of extraperitoneal injury with pelvic fractures treated by internal fixation, there is conflicting evidence about the need to repair the bladder in order to reduce the risk of infection [233,234].
Intraperitoneal ruptures should always be managed by surgical repair [193,196] because intraperitoneal urine extravasation can lead to peritonitis, intra-abdominal sepsis and death [195]. Abdominal organs should be inspected for possible associated injuries and urinomas must be drained if detected. Laparoscopic suturing of the intraperitoneal rupture is also possible [194].
4.3.5.2.2. Penetrating non-iatrogenic trauma
Penetrating bladder injury is managed by emergency exploration, debridement of devitalised bladder wall and primary bladder repair [202,203]. A midline exploratory cystotomy is advised to inspect the bladder wall and the distal ureters [202,230]. In gunshot wounds, there is a strong association with intestinal and rectal injuries, usually requiring faecal diversion [202,213]. Most gunshot wounds are associated with two transmural injuries (entry and exit wounds) and the bladder should be carefully checked for these two lesions [202]. In selected patients (haemodynamically stable without associated injuries), penetrating well-contained extraperitoneal bladder injuries probably can be safely managed non-operatively [235].
4.3.5.2.3. Iatrogenic bladder trauma
Perforations lacerations intra-operatively are primarily closed [236]. Bladder injuries not recognised during surgery or internal IBT should be managed according to their location. The standard of care for intraperitoneal injuries is surgical exploration and repair [223]. If surgical exploration is performed after TURB, the bowel must be inspected to rule out concomitant injury [207]. For extraperitoneal injuries, exploration is only needed for perforations complicated by symptomatic extravesical collections. It requires drainage of the collection, with or without closure of the perforation [237]. If bladder perforation is encountered during mid-urethral sling or transvaginal mesh procedures, sling re-insertion and urethral catheterisation (two to seven days) should be performed [238].
4.3.6. Follow-up
Continuous bladder drainage is required to prevent elevated intravesical pressure and to allow the bladder to heal [205,239]. Conservatively treated bladder injuries (traumatic or external IBT) are followed up by cystography to rule out extravasation and ensure proper bladder healing [193]. The first cystography is planned approximately ten days after injury [230]. In case of ongoing leakage, cystoscopy should be performed to rule out bony fragments in the bladder, and a second cystography is warranted one week later [193].
The optimal timing of catheter removal following iatrogenic bladder injury is unclear in current literature [240]. After operative repair of a simple injury in a healthy patient, the catheter can be removed after five to ten days without cystography [239,241]. In cases of complex injury (trigone involvement, ureteric re-implantation) or risk factors of impaired wound healing (e.g., steroids, malnutrition) cystography is advised [230,239]. For conservatively treated internal IBT, catheter drainage, lasting five to seven days, is proposed [208,211].
4.3.7. Summary of evidence and recommendations for bladder injury
| Summary of evidence | LE |
| The combination of pelvic fracture and visible haematuria is highly suggestive of bladder injury. | 3 |
| Cystography is the preferred diagnostic modality for non-iatrogenic bladder injury and for suspected IBT in the post-operative setting. | 3 |
| Cystography must be performed using retrograde filling of the bladder with a minimum volume of 300-350 mL of dilute contrast material. Passive bladder filling by clamping the urinary catheter during the excretory phase of CT or IVP is not sufficient to exclude bladder injury. | 3 |
| The risk of bladder perforation during mid-urethral sling operations for stress urinary incontinence is lower for the obturator route compared to the retropubic route. | 1a |
| Conservative treatment, which comprises of clinical observation, and continuous bladder drainage, is the standard treatment for an uncomplicated extraperitoneal injury due to blunt trauma. | 3 |
| In extraperitoneal bladder injury with either bladder neck involvement, bone fragments in the bladder wall, concomitant rectal or vaginal injury, or entrapment of the bladder wall, surgical intervention is necessary in order to decrease the risk of complications and to reduce recovery time. | 3 |
| Intraperitoneal bladder trauma is managed by surgical repair because intraperitoneal urine extravasation can lead to peritonitis, intra-abdominal sepsis, and death. | 3 |
| Conservative treatment is suitable for uncomplicated intraperitoneal injury during endo-urological procedures, in the absence of peritonitis and ileus. | 3 |
| In cases of complex injury (trigone involvement, ureteric re-implantation) or risk factors of impaired wound healing (e.g., steroids, malnutrition) cystography is advised after bladder repair. | 2a |
| Recommendations | Strength rating |
| Perform cystography in the presence of visible haematuria and pelvic fracture. | Strong |
| Perform cystography in case of suspected iatrogenic bladder injury in the post-operative setting. | Strong |
| Perform cystography with active retrograde filling of the bladder with dilute contrast (300-350 mL). | Strong |
| Perform cystoscopy to rule out bladder injury during retropubic sub-urethral sling procedures. | Strong |
| Manage uncomplicated blunt extraperitoneal bladder injuries conservatively. | Weak |
| Manage blunt extraperitoneal bladder injuries operatively in cases of bladder neck involvement and/or associated injuries that require surgical intervention. | Strong |
| Manage blunt intraperitoneal injuries by surgical exploration and repair. | Strong |
| Manage small uncomplicated intraperitoneal bladder injuries during endoscopic procedures conservatively. | Weak |
| Perform cystography to assess bladder wall healing after repair of a complex injury or in case of risk factors for wound healing. | Strong |
4.4. Urethral Trauma
4.4.1. Epidemiology, aetiology, and pathophysiology
The incidence of urethral injuries varies globally, with reported rates differing based on the region, healthcare infrastructure, and the specific population studied.
The incidence is more often reported in association with pelvic fractures, particularly in males, where the rate can reach up to 25% in such cases [242].
The nature of these injuries however can vary, including types such as crush injuries, bruising, lacerations, and transections. While these injuries are not life-threatening, they can lead to significant complications if not properly treated.
4.4.1.1. Anterior male urethral injury
The bulbar urethra is the most common site affected by blunt trauma. In bulbar injuries, the bulb is compressed against the pubic symphysis, resulting in damage of the urethra at the site of compression [243]. Possible mechanisms are straddle injuries or kicks to the perineum. A penile fracture can be complicated by a urethral injury in approximately 15% of cases, ranging between 1-38% depending on the aetiology [244-246]. Penetrating anterior injuries are rare and are usually caused by gunshot wounds, stab wounds, dog bites, impalement, or penile amputations [243]. Depending on the affected segment, penetrating injuries are usually associated with penile, testicular and/or pelvic injuries [247]. Insertion of foreign bodies is another rare cause of anterior urethral injury. It is usually a result of autoerotic stimulation or may be associated with psychiatric disorders. Management would depend on the location and nature of inserted device [248].
Iatrogenic injury is the most common type of urethral trauma [249]. The incidence of male urethral injury during transurethral catheterisation ranges from 6.2-13.4 per 1,000 catheters inserted [250,251]. Injuries can occur due to creation of a false passage by the tip of the catheter or inadvertent inflation of the anchoring balloon in the urethra [250]. The importance of catheter insertion training programmes [252-254] and the implementation of difficult urinary catheterisation protocols [255], to prevent urethral injury during transurethral catheterisation, have been demonstrated. Cystoscopic guidewire led catheter insertion, or use of a safety valve for balloon inflation may prevent urethral trauma in difficult catheterisation cases [254,256,257]. A SR of the use of hydrophilic coated catheters, in patients performing intermittent catheterisation, showed no clear benefit [258].
4.4.1.2. Posterior male urethral injuries
Blunt posterior urethral injuries are almost exclusively related to pelvic fractures and the risk increases with fracture configuration severity [259]. These injuries are referred to as pelvic fracture urethral injuries (PFUI) [243], and are mainly caused by road traffic accidents, motor vehicle crashes (68-84%) and falls from heights (6-25%) [260-262]. Pelvic fracture urethral injuries are divided into partial or complete ruptures [251,252]. In complete ruptures, there is a gap between the disrupted ends of the urethra, which fills up with scar tissue. There is no urethral wall in the scarred space and any lumen represents a fistulous tract between the urethral stumps [263]. Injuries of the bladder neck and prostate are rare and mostly occur at the anterior midline of both the bladder neck and prostatic urethra [264]. It is highly uncommon to find a complete transection of the bladder neck or an avulsion of the anterior part of the prostate [264]. Concomitant injuries to the head, thorax, abdomen and/or spine are frequent (up to 66%) [242].
Penetrating injuries of the pelvis, perineum, or buttocks (mainly gunshot wounds) can also damage the posterior urethra but are extremely rare in the civilian setting [259]. There is a high probability of associated injuries (approx. 90%), mainly intra-abdominal [202].
The associated injuries which occur with both blunt and penetrating posterior urethral injuries can be life-threatening, and if so, will govern the patient’s assessment and treatment [242]. Delayed morbidities of posterior urethral injuries include strictures, incontinence and erectile dysfunction, all of which may have a detrimental effect on the patient’s quality of life [265]. The proportion of patients with erectile dysfunction following PIFU unrelated to urethroplasty, is 34% [266]. Some previous studies have suggested that erectile dysfunction and incontinence may be higher in men undergoing EUR (endoscopic urethral realignment), while more recent evidence suggests that these complications are related to the underlying traumatic injury rather than the choice of management [267].
Iatrogenic injuries have been reported with transanal total mesorectal excision in 1-11% of cases. These injuries are usually partial and located at the membranous urethra [268].
4.4.1.3. Female urethral injuries
Birth related injuries to the female urethra are rare and consist of minor (peri)urethral lacerations during vaginal delivery. Motorcycle, bicycle and auto vs. pedestrian accidents are the main cause of blunt trauma, with younger population being particularly at risk [269,270]; however, PFUIs in females are rare and less common than in males [259] and associated with severe systemic injuries [270]. This is usually attributed to the flexibility provided by the vagina and the greater inherent elasticity of the female urethra [269]. It may also be the result of less severe and more frequent stable pelvic fractures in females [193,242]. In unstable pelvic fractures in females, a high suspicion for a urethral injury should be maintained [269]. Female urethral injuries are classified into two types: longitudinal or partial (most frequent) injuries and transverse or complete injuries [269]. Concomitant bladder or vaginal injury is possible; therefore, females are at risk of developing urinary incontinence and urethrovaginal fistula [242,269].
Insertion of a synthetic sub-urethral sling for the treatment of female stress urinary incontinence is complicated by an intra-operative urethral injury in 0.2-2.5% of cases [271] and is an important cause of iatrogenic urethral injury.
4.4.2. Evaluation
4.4.2.1. Clinical signs
Blood at the meatus is the cardinal sign, but the absence of it doesn’t rule out a urethral injury [193,242]. Inability to void (with a palpable distended bladder) is another classic sign and is often associated with a complete rupture [242,263]. Haematuria and pain on urination may be present in incomplete ruptures. Urinary extravasation and bleeding may result in scrotal, penile and/or perineal swelling and ecchymosis, depending on the location and extent of the trauma. The presentation of these clinical symptoms may be delayed (> 1 hour) [263].
Rectal examination should always be done to exclude an associated rectal injury (up to 5% of cases) and may reveal a ‘high-riding’ prostate, which is an unreliable finding [193,263]. Failure to detect a rectal injury can cause significant morbidity and even mortality. A rectal injury is suggested by blood on the examining finger and/or a palpable laceration [193]. Another sign of urethral injury is difficulty or inability to pass a urethral catheter [193,263].
A female urethral injury should be suspected from the combination of a (unstable) pelvic fracture with blood at the vaginal introitus, vaginal laceration, haematuria, urethrorrhagia, labial swelling, urinary retention, or difficulties passing a urethral catheter [193,265]. Vaginal examination is indicated to assess vaginal lacerations [193,265].
4.4.2.2. Urethrography
Retrograde urethrography (RUG) is the standard test in the early evaluation of a male urethral injury [193,272] and should be conducted by injecting 20-30 mL of contrast material while occluding the meatus. Films should be taken in a 30° oblique position. In patients with PFUI, it is important to move the X-ray beam to the 30° angle rather than the patient [242]. In an unstable patient, RUG should be postponed until the patient has been stabilised [193,202].
During RUG, any extravasation outside the urethra is pathognomonic for urethral injury [263]. A typical image for incomplete rupture shows extravasation from the urethra which occurs while the bladder is still filling. A complete rupture is suggested by massive extravasation without bladder filling [242]. Although RUG is able to reliably identify the site of injury (anterior vs. posterior), the distinction between a complete and partial rupture is not always clear [242,273]. Therefore, any proposed classification system based on RUG is not reliable [242,273]. In females, the short urethra and vulvar oedema make adequate urethrography nearly impossible [274].
Prior to deferred treatment, a combination of RUG and antegrade cysto-urethrography is advised to evaluate location and extent of the urethral injury, and to evaluate the competence of the bladder neck [242].
4.4.2.3. Cysto-urethroscopy
Flexible cysto-urethroscopy is a valuable alternative to diagnose an acute urethral injury and may distinguish between complete and partial rupture [272].
In females, where the short urethra often precludes adequate radiological visualisation, cysto-urethroscopy and vaginoscopy are the diagnostic modalities of choice [193,269]. If, prior to deferred treatment, the competence of the bladder neck is not clear upon antegrade cysto-urethrography, a suprapubic cystoscopy is advised [242].
4.4.2.4. Ultrasound and magnetic resonance imaging
In the acute phase, US should be used for guiding the placement of a suprapubic catheter [242]. In complex PFUIs, MRI before deferred treatment provides valuable additional information, which can help to determine the most appropriate surgical strategy [275,276]. This information includes a better estimation of the length of the distraction defect, degree of prostatic displacement and presence/absence of a false passage [275,276].
4.4.3. Disease Management
4.4.3.1. Male anterior urethral injuries
4.4.3.1.1. Immediate exploration and urethral reconstruction
This is indicated for penile fracture related injuries [277] and non-life-threatening penetrating injuries [265]. Small lacerations can be repaired by simple closure [245]. Complete ruptures without extensive tissue loss are treated with anastomotic repair [245,247]. Only 2% of cases will develop a urethral stricture after immediate urethral reconstruction for penile fracture [277]. In the case of longer defects or apparent infection (particularly bite wounds), a staged repair with urethral marsupialisation is needed [272]. Consider giving peri- and post-operative antibiotic treatment for penetrating injuries according to local guidelines [278].
Performing immediate anterior urethroplasty in blunt injuries is highly controversial and, should only be performed by a dedicated urethral surgeon [279,280].
4.4.3.1.2. Urinary diversion
Blunt anterior urethral injuries are associated with spongiosal contusion. Evaluation of the limits of urethral debridement in the acute phase might be difficult and as a consequence, it is reasonable to start with urinary diversion only [272].
If urinary diversion is performed, the therapeutic options are suprapubic diversion or a trial of early endoscopic re-alignment with transurethral catheterisation [272]; there is conflicting evidence as to which intervention is superior [279,281,282]. A retrospective case series of 44 patients comparing early realignment versus suprapubic tube placement, shows no difference in stricture formation [283].
Urinary diversion is maintained for one to two weeks for partial ruptures and three weeks for complete ruptures [272,281]. A review of 49 Chinese studies (1,015 patients), reported a 57% (range: 0-100%) success rate for endoscopic re-alignment of blunt anterior injuries [279]. The wide range in success rate most likely reflects a mix of partial and complete ruptures which was not further specified in the review. For complete ruptures, urinary diversion on its own is unlikely to result in a successful outcome (0-25% patency rate) [281,282].
Transurethral or suprapubic urinary diversion are treatment options for iatrogenic or life-threatening penetrating injuries [265,284]. Minor iatrogenic urethral injuries and urethral contusions do not require urinary diversion [3].
4.4.3.2. Male posterior urethral injuries
4.4.3.2.1. Emergency room management
As these injuries are usually associated with other severe injuries, resuscitation and immediate treatment of life-threatening injuries have absolute priority [242]. Penetrating injuries especially have a very high likelihood of associated injuries requiring immediate exploration [202,285]. There is no urgency to treat the urethral injury, and urinary diversion is not essential during the first hours after trauma [263]; however, it is preferable to establish early urinary diversion to:
- monitor urinary output, since this is a valuable sign of the haemodynamic condition and the renal function of the patient;
- treat symptomatic retention if the patient is still conscious;
- minimise urinary extravasation and its secondary effects, such as infection and fibrosis [242].
Insertion of a suprapubic catheter is an accepted practice in urgent situations [263,285,286]. However, insertion of a suprapubic catheter is not without risk, especially in the unstable trauma patient where the bladder is often displaced by a pelvic haematoma or because of poor bladder filling due to haemodynamic shock or concomitant bladder injury. In these circumstances, an attempt at urethral catheterisation can be carried out by experienced personnel. It is extremely unlikely that the gentle passage of a urethral catheter will do any additional damage [242]. If there is any difficulty, a suprapubic catheter should be placed under US guidance or under direct vision, for example, during laparotomy for associated injuries [242]. Suprapubic catheter placement does not increase the risk of infectious complications in patients undergoing internal fixation to stabilise a pelvic fracture [287]. Therefore, the assertion that suprapubic catheter placement would increase the risk of orthopaedic hardware infection and subsequent explantation is not justified [287].
4.4.3.2.2. Early urethral management (less than six weeks after injury)
For partial injuries, urinary diversion (suprapubic or transurethral) is sufficient as these injuries can heal without significant scarring or obstruction [263,265]. A complete injury will likely not heal, and formation of an obliterated segment is almost inevitable in case of suprapubic diversion alone [263,265,286].
4.4.3.2.2.1. Early re-alignment
Early re-alignment can be performed when a stable patient is on the operating table for other surgery or as a stand-alone procedure in the absence of concomitant injuries [202,288]. In a partial injury, re-alignment, and transurethral catheterisation avoids extravasation of urine in the surrounding tissues reducing the inflammatory response. In complete injuries, the aim of re-alignment is to correct severe distraction injuries rather than to prevent a stricture [265,267,289].
Re-alignment can be done by an open or endoscopic technique [289,290]. The open technique is associated with longer operation times, more blood loss and longer hospital stays; as such, endoscopic re-alignment is now preferred [279]. Using a flexible/rigid cystoscope and biplanar fluoroscopy, a guidewire is placed inside the bladder under direct visual control, over this, a catheter is placed. If necessary, two cystoscopes can be used: one retrograde (per urethra) and one antegrade (suprapubic route through the bladder neck) [242]. The duration of catheterisation is three weeks for partial and six weeks for complete ruptures with voiding urethrography upon catheter removal [242]. It is important to avoid traction on the balloon catheter as it can damage the remaining sphincter mechanism at the bladder neck [242].
Data from an RCT demonstrated no difference in the urethral stricture rate for complete rupture PFUI [267]. There is also no evidence that early re-alignment increases the risk of urinary incontinence (4.7-5.8%) or erectile dysfunction (16.7-20.5%) [290,291].
Potential benefit of early re-alignment is that when a stricture occurs it will be shorter and therefore, easier to treat. For short, non-obliterative strictures following re-alignment, direct vision urethrotomy can be performed. Approximately 50% of strictures after endoscopic re-alignment can be treated endoscopically [289]. However, repetitive endoscopic procedures in case of stricture formation might delay the time to definitive cure and can increase the incidence of adverse events (false passage, abscess formation) [292,293]. In light of this, repetitive endoscopic treatments after failed re-alignment are not recommended; instead, urethroplasty must be performed.
A retrospective review found a shorter stricture length after early (open) re-alignment and as a consequence, a tendency for less complex manoeuvres to be needed to allow for a tension-free anastomosis during urethroplasty [261]. On the other hand, another retrospective review, reported an equal stricture length and no greater facilitation of urethroplasty after failed endoscopic re-alignment compared to suprapubic diversion only [292]. The proposed benefit is thus highly questionable. Furthermore, there is conflicting evidence as to whether failed early re-alignment jeopardises the success of definitive urethroplasty [242].
Differences between series in the rates of incontinence, impotence and re-stricture can be explained by differences in patient selection (severe vs. less severe trauma), a mix of partial and complete ruptures, and differences in follow-up duration. Furthermore, these differences make the comparison with other techniques difficult, especially with urethroplasty [193,289].
4.4.3.2.2.2. Early urethroplasty
Immediate urethroplasty within 48-hours after injury is difficult because of poor visualisation and the inability to accurately assess the degree of urethral disruption, due to extensive swelling and ecchymosis, which may result in extensive unjustified urethral debridement. Another problem is the risk of severe bleeding (average 3 L) following entry into the pelvic haematoma [242]. In addition, with high rates of erectile dysfunction (23%), urinary incontinence (14%) and re-stenosis (54%), urethroplasty within 48 hours is not indicated [242].
Early urethroplasty can be performed after two days and up to six weeks after the initial injury, if associated injuries have been stabilised, the distraction defect is short, the perineum is soft and the patient is able to lie down in the lithotomy position [294,295]. This avoids a long period of suprapubic diversion with its discomfort and complications [294,295]. As the results (complications, stricture recurrence, incontinence, and erectile dysfunction) are equivalent to delayed urethroplasty [295-297], early urethroplasty might be an option for patients fulfilling the above-mentioned criteria.
Lacerations (blunt or penetrating) at the bladder neck and prostatic urethra are a specific entity: they would never heal spontaneously, could cause local cavitation (presenting a source of infection) and compromise the intrinsic sphincter mechanism (with increased risk of urinary incontinence), they must be reconstructed as soon as possible [264]. For penetrating injuries with severe lacerations to the prostate, radical prostatectomy with bladder neck sparing could be required [285].
4.4.3.2.3. Deferred management (greater than three months after injury)
The standard treatment remains deferred urethroplasty [298]. In the case of a complete rupture, treated with an initial period of three months suprapubic diversion, obliteration of the posterior urethra is almost inevitable [263]. Endoscopic treatment of a complete obliteration is not successful and risky [242]. After at least three months of suprapubic diversion, the pelvic haematoma is nearly always resolved, the prostate has descended into a more anatomical position, the scar tissue has stabilised [294] and the patient is clinically stable and able to lie down in the lithotomy position [272,294]. Associated life-threatening injuries often preclude early management of penetrating membranous urethral injuries. In those cases, suprapubic diversion with delayed urethroplasty is also advised [19,28,30]. Perineal anastomotic repair is the surgical technique of choice, but a combined abdominoperineal approach would be necessary in rare cases of concomitant bladder neck injury, recto-urethral fistula, multiple prior attempts to repair, or long distance between proximal and distal urethral stumps [299,300].
An extensive overview of deferred urethroplasty can be found in the Urethral Strictures Guidelines including the need for extensive follow-up [301].
4.4.3.2.4. Iatrogenic posterior injuries
Urethral defects during transanal total mesorectal excision were repaired by direct suture repair via a transperineal approach in a small case series (n=32). Despite direct repair, 26% developed complications including urethral stricture, urethral dehiscence, recto-urethral fistula, and recto-perineal fistula. No evidence on other strategies is available [268].
4.4.3.3. Female urethral injuries
Emergency room management of PFUIs in females is the same as in males (section 4.4.3.2.1); however, subsequent management differs. Treatment options are [269]:
- Early realignment: This is associated with a high stricture and fistula rate.
- Early repair (seven days or less): Complication rate is the lowest with early repair; therefore, this strategy is preferred once the patient is haemodynamically stable [265,269].
- Delayed repair (more than seven days): Delayed repair often requires complex abdominal or combined abdominal-vaginal reconstruction with elevated risk of urinary incontinence and vaginal stenosis.
The approach (vaginal, abdominal or combined) for early repair depends on the location of the injury [269]. Proximal and mid-urethral disruptions require immediate exploration and primary repair using the retropubic and transvaginal routes, respectively, with primary suturing of the urethral ends or urethral laceration. Concomitant vaginal lacerations are repaired (two-layer closure) trans vaginally at the same time [269]. Distal urethral injuries can be left hypospadiac since they do not disrupt the sphincter mechanism, but a concomitant vaginal laceration must be closed [193,274]. In case of urethral injury during synthetic sub-urethral sling insertion, immediate repair is warranted with abandonment of sling insertion [271].
Table 4.4.1: Complication rates for different treatment strategies for PFUIs in females [269]
| Type of repair | Stricture (%) | Fistula (%) | Incontinence (%) | Vaginal stenosis (%) | Need for permanent urinary diversion (%) |
| Early realignment | 59 | 13 | 0 | 0 | 0 |
| Early repair | 3 | 6 | 9 | 0 | 3 |
| Delayed repair | 3 | 4 | 31 | 4 | 7 |
4.4.4. Summary of evidence and recommendations for the evaluation and management of urethral trauma
| Summary of evidence | LE |
| Implementing training programmes on urinary catheter insertion for personnel involved with urethral catheterisation significantly improves the rate of catheter-related complications. | 2b |
| In males, a urethral injury is detected as contrast extravasation during urethrography or as a mucosal laceration during cysto-urethroscopy. | 3 |
| As opposed to cysto-urethroscopy, voiding cysto-urethrography will miss a female urethral injury in approximately 50% of cases. | 3 |
| Transurethral or suprapubic urinary diversion are the treatment options for iatrogenic injuries. | 3 |
| With urinary diversion (suprapubic or transurethral catheter) satisfactory urethral luminal re-canalisation may occur after partial blunt anterior urethral ruptures. | 3 |
| If PFUIs are associated with life-threatening injuries, urethral management has no priority and urinary diversion with either urethral or suprapubic catheterisation is sufficient initially. | 3 |
| With early endoscopic re-alignment the stricture rate is reduced to 44-49% without increased risk of incontinence or erectile dysfunction. | 3 |
| Repetitive endoscopic treatments after failed re-alignment delay the time to definitive cure and increase the incidence of adverse events. | 3 |
| For partial posterior injuries, urinary diversion (suprapubic or transurethral) is sufficient as these injuries might heal without significant scarring or obstruction. | 3 |
| Immediate urethroplasty (< 48 hours) in male PFUI is associated with a higher risk of bleeding, stricture, incontinence, and impotence rates compared to delayed urethroplasty. | 3 |
| In selected patients for male PFUI, early urethroplasty (two days to six weeks) is associated with similar stricture, incontinence and impotence rates compared to delayed urethroplasty. | 3 |
| Suprapubic diversion with delayed urethroplasty in male PFUI with complete urethral disruption is associated with an 86% stricture free success rate and with no significant impact on erectile function and urinary continence. | 2a |
| Early repair in female PFUI has the lowest complication rate. | 3 |
| Recommendations | Strength rating |
| Provide appropriate training to reduce the risk of traumatic catheterisation. | Strong |
| Evaluate male urethral injuries with flexible cysto-urethroscopy and/or retrograde urethrography. | Strong |
| Evaluate female urethral injuries with cysto-urethroscopy and vaginoscopy. | Strong |
| Treat iatrogenic anterior urethral injuries by transurethral or suprapubic urinary diversion. | Strong |
| Treat partial blunt anterior urethral injuries by suprapubic or urethral catheterisation. | Strong |
| Treat pelvic fracture urethral injuries (PFUIs) in haemodynamically unstable patients initially by transurethral or suprapubic catheterisation. | Strong |
| Perform early endoscopic re-alignment in male PFUIs when feasible. | Weak |
| Do not repeat endoscopic treatments after failed re-alignment for male PFUI. | Strong |
| Treat partial posterior urethral injuries initially by suprapubic or transurethral catheter. | Strong |
| Do not perform immediate urethroplasty (< 48 hours) in male PFUIs. | Strong |
| Perform early urethroplasty (two days to six weeks) for male PFUIs with complete disruption in selected patients (stable, short gap, soft perineum, lithotomy position possible). | Weak |
| Manage complete posterior urethral disruption in male PFUIs with suprapubic diversion and deferred (at least three months) urethroplasty. | Strong |
| Perform early repair (within seven days) for female PFUIs (not delayed repair or early re-alignment). | Strong |
4.4.5. Treatment algorithms
Management of anterior and posterior urethral injuries in men.
Figure 4.4.1: Management of anterior urethral injuries in men
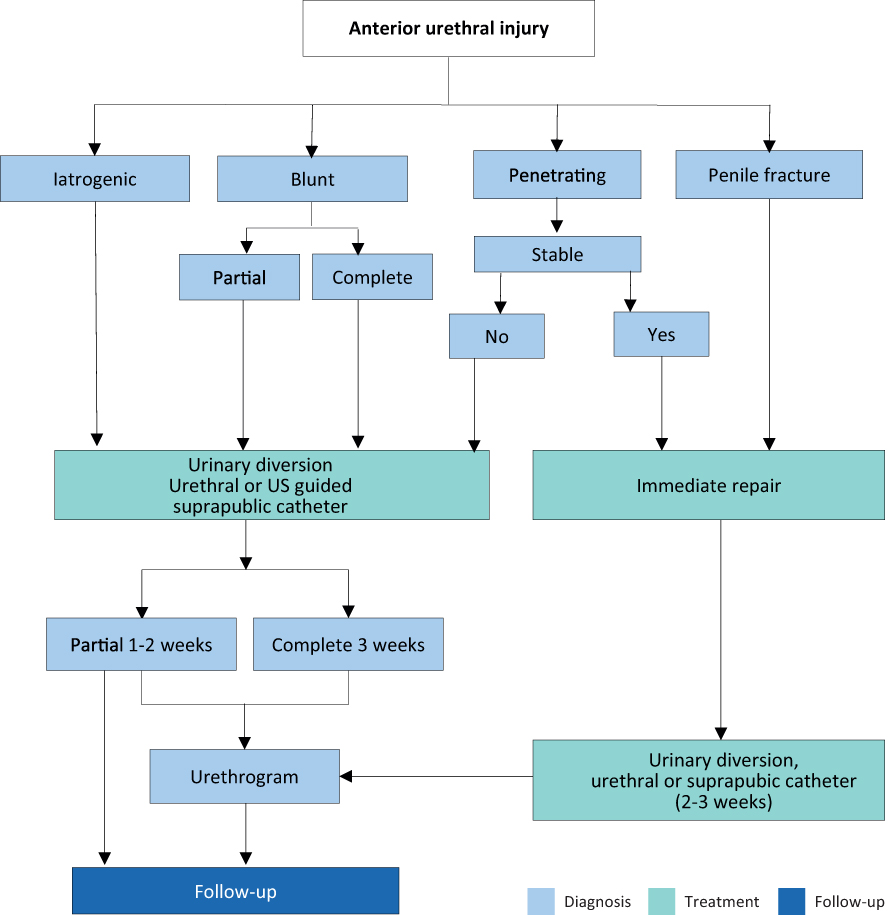
Figure 4.4.2: Management of posterior urethral injuries in men

RUG = retrograde urethrography; DVIU = direct visual internal urethrotomy.
4.5. Genital Trauma
4.5.1. Epidemiology, aetiology and pathophysiology
Of all urological injuries, 33-66% involve the external genitalia [302]. Genital trauma is much more common in males than in females, especially between the ages of 15 and 40 years. This is due to anatomical differences, increased frequency of road traffic accidents and increased participation in physical sports, war and crime [303]. The risk of associated injuries to neighbouring organs (bladder, urethra, vagina, rectum, and bowel), after blunt trauma is higher in females than in males.
Genital trauma is commonly caused by blunt injuries (80%). In males, blunt genital trauma frequently occurs unilaterally with approximately 1% presenting as bilateral scrotal or testicular injuries [304]. Any kind of contact sport, without the use of protective aids, may be associated with genital trauma. Off-road cycling, motor biking (especially on motorbikes with a dominant petrol tank), rugby, football and hockey are all activities associated with blunt testicular trauma [305-308]. Penetrating injuries are most commonly caused by firearms (75.8%) with the majority requiring surgical intervention [309,310].
Accidents during sexual intercourse can also cause genital trauma; men of younger age are the most affected. The major pathologies are penile fractures, strangulation, necrosis, and associated injuries from various sexual practices [311,312].
The most important presentation of blunt penile trauma is penile fracture. The common causes are sexual intercourse, forced flexion (taqaandan), masturbation and rolling over [313]. It has also been reported that penile fracture patients have a significantly higher rate of substance abuse [314]. The usual mechanism of injury is when the penis slips out of the vagina and strikes against the symphysis pubis or perineum. Sixty per cent of cases occur during consensual intercourse [315], with penile fracture more likely in certain positions [316]. Penile fracture is caused by rupture of the cavernosal tunica albuginea and may be associated with subcutaneous haematoma and lesions of the corpus spongiosum or urethra in 10-22% [317-319].
Although animal bites are common, bites injuring the external genitalia are rare. Wounds are usually minor but have a risk of wound infection.
Gunshot injuries to the external genitalia are relatively uncommon and are usually not life-threatening; however, they can have a significant impact on quality of life. About 40-60% of all penetrating genito-urinary lesions involve the external genitalia [320,321], 35% of these are gunshot wounds [304]. In a series of wartime injuries, the majority were caused by improvised explosive devices and other explosive ordinance, while smaller numbers of injuries were due to gunshot injuries [322]. In both males and females, penetrating injuries affect multiple organs in 70% of patients. In males, penetrating scrotal injuries affect both testes in 30% of cases compared with 1% in blunt injuries [304,323]. Self-mutilation of the external genitalia has also been reported in psychotic patients [324]. Genital burns are rare in isolation and are usually due to industrial flames or chemicals [325]. Both male and female genital piercings increase the risk for genital trauma [326].
Traumatic dislocation of the testicle rarely occurs and is most common in victims of road traffic accidents [327-330]. Bilateral dislocation of the testes has been reported in up to 25% of cases [328]. Testicular rupture is found in approximately 50% of cases of direct blunt scrotal trauma [331,332]. It may occur under intense compression of the testis against the inferior pubic ramus or symphysis, resulting in a rupture of the tunica albuginea. A force of approximately 50 kg is necessary to cause testicular rupture [333].
Coital injury of the female genital tract can happen during consensual sexual intercourse. Up to 35% of all genital injuries in women are sustained during their first sexual contact. The most frequently found injuries are lacerations [334]. Blunt trauma to the vulva is rarely reported and usually presents as a large haematoma. The incidence of traumatic vulvar haematomas after vaginal deliveries has been reported as one in 310 deliveries [335]. The presence of a vulvar haematoma is closely related to an increased risk of associated vaginal, pelvic, or abdominal injuries [336,337]. Blunt injuries of the vulva and vagina are associated with pelvic trauma in 30%, after consensual intercourse in 25%, following sexual assault in 20%, and other blunt trauma in 15% [338].
4.5.2. Diagnostic evaluation
Penile fracture is associated with a sudden cracking or popping sound, pain and immediate detumescence. Local swelling of the penile shaft develops quickly, due to enlarging haematoma [244]. Bleeding may spread along the fascial layers of the penile shaft and extend to the lower abdominal wall if Buck’s fascia is also ruptured. Sometimes, the rupture of the tunica may be palpable. Failure to diagnose false penile fractures may lead to unnecessary operations. The absence of a cracking sound, slow detumescence, penile deviation, and ecchymosis of the shaft are highly sensitive signs for false penile fractures [339].
Testicular rupture is associated with immediate pain, nausea, vomiting, and sometimes fainting. The hemiscrotum is tender, swollen, and ecchymotic. The testis itself may be difficult to palpate.
Blunt vulvar or perineal trauma in women may be associated with bleeding, pain and voiding problems, bladder catheterisation is usually required.
In genital trauma, a urinalysis should be performed. The presence of visible haematuria requires a retrograde urethrogram in males. In females, flexible or rigid cystoscopy is recommended to exclude urethral and bladder injury [336,338]. In women with genital injuries and blood at the vaginal introitus, further gynaecological investigation is needed [336].
In cases of suspected penile fracture cavernosography, US or contrast-enhanced MRI [313,340-342] can identify lacerations of the tunica albuginea in unclear cases [343] or provide reassurance that the tunica is intact. Magnetic resonance imaging is superior to US in diagnosing penile fracture [344,345]. If a concomitant urethral injury is suspected, manage as outlined in section 4.4.
Intra-operative flexible cystoscopy can be performed during surgical exploration of penile fracture to rule out associated urethral injuries [263,264].
Ultrasound should be performed to determine intra- and/or extra-testicular haematoma, testicular contusion, or rupture [332,346-354]. However, the literature is contradictory as to the usefulness of US compared to clinical examination alone. Some studies have reported convincing findings with a specificity of up to 98.6% [355]. Heterogeneous echo pattern of the testicular parenchyma with the loss of contour definition is a highly sensitive and specific radiographic finding for testicular rupture [344]. Others reported poor specificity (78%) and sensitivity (28%) for the differentiation between testicular rupture and haematocele, while accuracy is as low as 56% [347]. Colour Doppler-duplex US may provide useful information when used to evaluate testicular perfusion. If scrotal US is inconclusive, testicular CT or MRI may be helpful [356]; however, these techniques did not specifically increase the detection rates of testicular rupture [357].
4.5.3. Disease management
4.5.3.1. Animal bites
Local wound management depends on the extent of tissue destruction. Antibiotics should be prescribed in accordance with local resistance patterns [358]. The possibility of rabies infection must be considered, considering the geographical location, animal involved, specific nature of the wound and the type of attack (provoked/unprovoked). Elderly and immunosuppressed patients should be vaccinated with human rabies immunoglobulin and human diploid cell vaccine [359,360].
4.5.3.2. Human bites
In cases of human bites, apart from wound management, infection should be considered since transmission of viral diseases may occur, Hepatitis B vaccine/immunoglobulin and/or immunodeficiency virus (HIV) post-exposure prophylaxis should be offered. For further details, see Guidelines for the Management of Human Bite Injuries [361].
4.5.3.3. Blunt penile trauma
Blunt trauma to the flaccid penis does not usually cause tearing of the tunica. Subcutaneous haematoma after sexual intercourse, without associated rupture of the cavernosal tunica albuginea, does not require surgical intervention. In these cases, non-steroidal analgesics and ice-packs are recommended [362].
4.5.3.4. Penile fracture
The thickness of the tunica albuginea in the flaccid state (approximately 2 mm) decreases in erection to 0.25-0.5 mm and is therefore more vulnerable to traumatic injury [355,363]. When a penile fracture is diagnosed, surgical intervention with closure of the tunica albuginea is recommended; it ensures the lowest rate of negative long-term sequelae and has no negative effect on the psychological wellbeing of the patient [364]. The approach is usually through a circumferential incision proximal to the coronal sulcus which enables complete degloving of the penis. Increasingly, local longitudinal incisions centred on the area of fracture or ventral longitudinal approaches are currently used [365]. A recent SR on the management of penile fractures concluded that immediate repair should be within 24 hours of presentation [366]; however, delayed presentation should not prevent exploration [316]. Further localisation may be gained with a flexible cystoscopy performed prior to incision, if urethral trauma is suspected and eventually proven [244]. Surgical closure of the tunica should be carried out using absorbable sutures.
4.5.3.5. Penetrating penile trauma
In penetrating penile trauma non-operative management is recommended for small superficial injuries with intact Buck’s fascia [320]. In more significant penetrating penile injuries, surgical exploration and debridement of necrotic tissue is recommended. Even in extended injuries of the penis, primary alignment of the disrupted tissues may allow for acceptable healing because of the robust penile blood supply [324].
The principles of care are debridement of devitalised tissue, with the preservation of as much viable tissues as possible, haemostasis, diversion of urine in selected cases and the removal of foreign bodies. Tissues of questionable viability may be left for subsequent definitive surgery.
The surgical approach depends upon the site and extent of the injury, but a subcoronal incision with penile degloving usually gives good exposure. Initially, a defect in the tunica albuginea should be closed after copious irrigation. If there has been too much tissue loss, the defect can be repaired either immediately or after delay with a graft (autologous, xenograft or artificial).
The elasticity of genital skin means it is usually possible to manage the loss of a moderate amount of penile skin; however, management is more difficult in extensive injuries with significant skin loss. The tissue chosen for reconstruction following trauma needs to provide good coverage and must be suitable for reconstruction. Skin grafts with thickness of at least 0.4 mm should be used in order to reduce the risk of contraction [324]. Full-thickness skin grafting onto the penile shaft gives less contracture, a better cosmetic appearance and more resistance to trauma during intercourse, when re-established [362]. The donor site may be taken from the abdomen, buttock, thigh, or axilla and is chosen according to surgeon’s preference and the pattern of injury. In cases of extensive destruction of deeper tissues, or if later prosthetic placement is being considered, skin flaps, with their secure vascular supply, can be used.
4.5.3.6. Penile avulsion injuries and amputation
Acute management involves resuscitation of the patient, and preparation for surgical re-implantation of the penis if it has been recovered and is not too badly damaged. Surgical re-implantation should be considered for all patients and should be performed within 24 hours of amputation [367].
The severed penis should be washed with sterile saline, wrapped in saline-soaked gauze, placed in a sterile bag, and immersed in iced water. The penis must not come into direct contact with the ice. A pressure dressing or a tourniquet should be placed around the penile stump to prevent excessive blood loss. Re-attachment can be achieved in a non-microsurgical way, but a microsurgical approach, with anastomosis of the corpora cavernosa, the urethra, the dorsal penile arteries, the dorsal vein, and the dorsal nerves, is preferred. The cavernosal arteries are generally too small to anastomose. The fascia and skin are closed in layers and both a urethral and a suprapubic catheter are placed [368].
If the severed penis cannot be found, or is unsuitable for re-attachment, then the end should be closed as it is done in partial penectomy. Later reconstruction may be employed to lengthen the penis (e.g., suspensory ligament division and V-Y plasty, pseudo-glans formation with split-thickness skin grafting, etc.). A delayed major reconstructive procedure, i.e. phalloplasty (either radial artery or pubic), is sometimes required for injuries which leave a very small or non-functioning penile stump [367].
4.5.3.7. Testicular dislocation
It can be either a subcutaneous dislocation with epifascial displacement of the testis or an internal dislocation. In the latter, the testis is positioned in the superficial external inguinal ring, inguinal canal or abdominal cavity. Traumatic dislocation of the testis is treated by manual replacement and secondary orchidopexy. If primary manual reposition cannot be performed, immediate orchidopexy is indicated.
4.5.3.8. Haematocoele
Conservative management is recommended in haematoceles smaller than three times the size of the contralateral testis [369]. In large haematoceles, non-operative management can fail, and delayed surgery (more than three days) is often required. Patients with large haematoceles have a higher rate of orchiectomy than patients who undergo early surgery, even in non-ruptured testes [304,324,331,370,371]. Early surgical intervention results in preservation of the testis in more than 90% of cases compared to delayed surgeries which result in orchiectomy in 45-55% of patients [331]. In addition, non-operative management is also associated with prolonged hospital stays. Therefore, large haematoceles should be treated surgically, irrespective of the presence of testicular contusion or rupture. At the very least, the blood clot should be evacuated from the tunica vaginalis sac to relieve disability and hasten recovery.
4.5.3.9. Testicular rupture
It is essential to surgically explore patients with equivocal findings, whenever imaging studies cannot definitively exclude testicular rupture. This involves exploration with evacuation of blood clots and haematoma, excision of any necrotic testicular tubules and closure of the tunica albuginea.
4.5.3.10. Penetrating scrotal trauma
Penetrating injuries to the scrotum require surgical exploration with debridement of non-viable tissue. Depending on the extent of the injury, primary reconstruction of the testis and scrotum can usually be performed. In complete disruption of the spermatic cord, re-alignment without vaso-vasostomy may be considered if surgically feasible [372]. Staged secondary microsurgical vaso-vasostomy can be performed after recovery, although only a few cases have been reported [372]. If there is extensive destruction of the tunica albuginea, mobilisation of a free tunica vaginalis flap can be performed for testicular closure. If the patient is unstable or reconstruction cannot be achieved, orchiectomy is indicated.
Extended laceration of scrotal skin requires surgical intervention for skin closure. Due to the elasticity of the scrotum, most defects can be primarily closed, even if the lacerated skin is only minimally attached to the scrotum [324]. Local wound management with extensive initial wound debridement and washout is important for scrotal convalescence. In the case of extensive loss of genital tissue, e.g., improvised explosive device blast injury, complex and staged reconstructive surgical procedures are often required [322]. Military testicular salvage rates increased over the last decades due to improvements of medical services (up to 67.6%) [373].
Table 4.5.1: Summary of key points for penile fracture and testicular trauma
| Summary of key points: |
| Penile fracture |
| The most common causes of penile fracture are sexual intercourse, forced flexion, masturbation and rolling over. |
| Penile fracture is associated with a sudden cracking or popping sound, pain, immediate detumescence and local swelling. |
| MRI is superior to all other imaging techniques in diagnosing penile fracture. |
| Management of penile fracture is surgical intervention with closure of the tunica albuginea. |
| Testicular Trauma |
| Blunt testicular injury may occur under intense compression of the testis against the inferior pubic ramus or symphysis, resulting in a rupture of the tunica albuginea. |
| Testicular rupture is associated with immediate pain, nausea, vomiting, and sometimes fainting. |
| Scrotal US is the preferred imaging modality for the diagnosis of testicular trauma. |
| Surgical exploration in patients with testicular trauma ensures preservation of viable tissue when possible. |
4.5.4. Complications
The possibility of complications from genital trauma, including psychological effects, erectile dysfunction, urethral stricture, and infertility, is high. In patients with a history of penile fracture post-operative complications were reported in up to 20% of cases, development of plaques or nodules following surgery, post-operative curvature formation and erectile dysfunction occur in 13.9%, 2.8% and 1.9% of patients, respectively [313]. Post-surgical erectile dysfunction is more common in patients > 50 years and those with bilateral corporal involvement [374]. Skin necrosis is rare [316]. The tear size of the tunica albuginea is a parameter which may affect long-term follow-up results [375].
Conservative management of penile fracture increases complications, such as penile abscess, missed urethral disruption, penile curvature, and persistent haematoma requiring delayed surgical intervention [376]. Late complications after conservative management were fibrosis and angulations in 35% and impotence in up to 62% [315,377].
Post-operative complications were reported in 8% of patients who underwent testicular repair after penetrating trauma [320]. Despite good management and regular follow-up of external genital gunshot wounds, such wounds are fraught with the possibility of complications such as erectile dysfunction, urethral stricture, and infertility. Delayed complications include chronic pain and testicular atrophy. Haematoceles initially treated non-operatively may eventually need delayed surgery if they develop infection or undue pain. Genital injuries are rarely life threatening, but fertility and testosterone production often become the male trauma patient’s chief concern once acute issues are resolved [378].
4.5.5. Follow-up
In patients with genital trauma follow-up should focus on diagnosis of and therapy for late complications. Erectile dysfunction, urethral stricture and assessment of fertility are the main concerns [319,379].
4.5.6. Summary of evidence and recommendations for evaluation and management of genital trauma.
| Summary of evidence | LE |
| A concomitant urethral injury complicates penile fractures and requires specialised management. | 3 |
| Ultrasound can determine intra- and/or extra-testicular haematoma, testicular contusion, or rupture with heterogeneous echo pattern parenchyma and loss of contour definition a highly sensitive and specific finding. | 3 |
| Surgical treatment of penile fracture ensures the lowest rate of negative long-term sequelae on functional and psychological wellbeing of the patient. | 3 |
| In patients with testicular rupture or equivocal imaging, surgical exploration can secure preservation of viable tissue. | 3 |
| Recommendations | Strength rating |
| Exclude urethral injury in the case of penile fracture. | Strong |
| Perform ultrasound (US) for the diagnosis of testis trauma. | Strong |
| Treat penile fractures surgically, with closure of tunica albuginea. | Strong |
| Explore the injured testis in all cases of testicular rupture and in those with inconclusive US findings. | Strong |