The role of robotics in functional urology (Part 2)
This is part 2 of the article on the use of robotic surgery in functional urology. Read Part 1 here.
(1) Department of Urology, Jagiellonian University Medical College, Krakow, Poland
(2) Department of Urology, Royal Hallamshire Hospital, Sheffield, UK
3. Incontinence
Colposuspension
Although once considered the gold standard, the use of Burch colposuspension declined with the introduction of the mid-urethral tape. However, the technique has seen a resurgence in recent years due to the well-publicised issues with transvaginal mesh. Robotic Burch colposuspension was first described in 2015, followed by a case report published in 2017.
Apart from these isolated reports, the evidence remains limited. A pilot study comparing robotic hysterectomy with robotic colposuspension to open hysterectomy and colposuspension found no significant differences in continence rates between the two groups, although the inclusion of concomitant hysterectomy could be a confounding factor. While long-term data is still needed, existing literature suggests that laparoscopic colposuspension, when performed by experienced surgeons, yields similar outcomes to the open procedure.
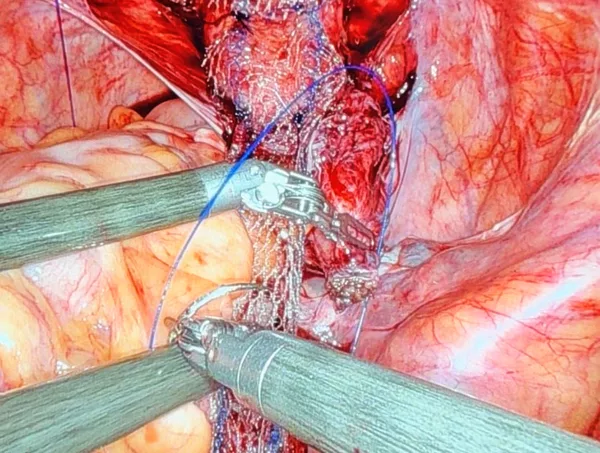
Artificial urinary sphincter (AUS)
In men with post-prostatectomy incontinence, AUS is typically placed through a perineal approach at the bulbar urethra. Bladder neck placement of the AUS is indicated for male neurogenic patients with a sphincter deficit and for women with stress urinary incontinence, usually following failed other surgical interventions.
The first report of robotic AUS placement in men with neurogenic stress incontinence was published in 2013. In this study, six male patients underwent the procedure, with a median operating time of 195 minutes, no significant blood loss, and no major complications. At a median follow-up of 13 months, all patients were continent, with no signs of erosion or device malfunction. Although these findings are promising, another series involving four men reported persistent incontinence in two patients.
Robotic AUS implantation in women has also been described by several groups, with evidence of reduced operative time, blood loss, and length of stay compared to open surgery, while achieving similar functional outcomes. However, some series have reported a high incidence of visceral injury, such as to the vagina or bladder, with rates as high as 4 out of 11 cases. There is a need for further randomised, prospective studies to establish the safety and efficacy of the robotic approach over open surgery. Technical expertise will be crucial, as these cases are often complicated by prior surgeries that result in intra-pelvic adhesions.
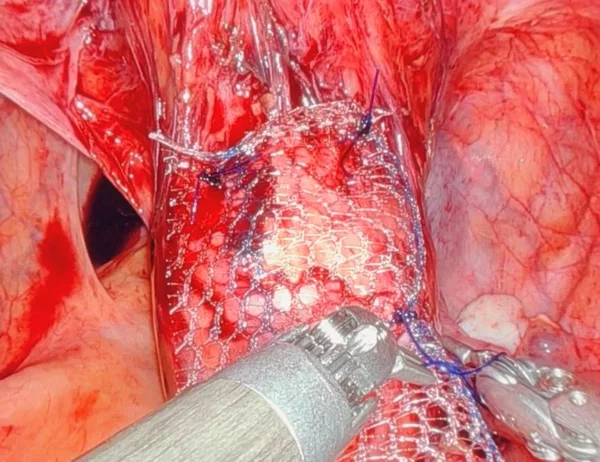
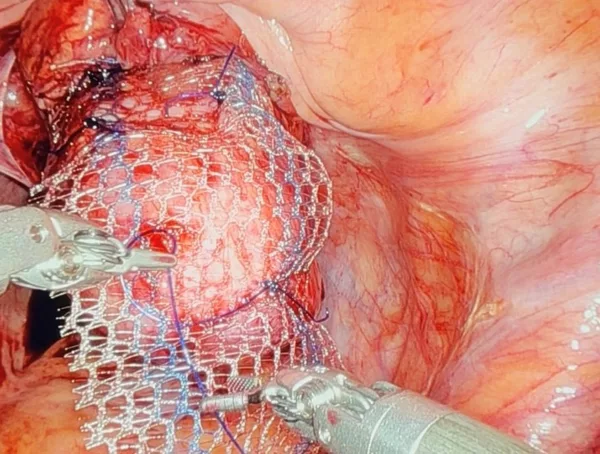
4. Prolapse
Sacrocolpopexy
Abdominal sacrocolpopexy is considered the gold standard for treating apical and multicompartment prolapse. Robot-assisted sacrocolpopexy has been widely reported and studied. A meta-analysis of 1,488 cases from 27 studies conducted between 2006 and 2013 demonstrated that the procedure is safe and effective, with an objective cure rate ranging from 84% to 100%, a recurrence rate of 6.4%, and a reoperation rate of 3.3%. Follow-up periods ranged from 3 to 25 months. The robotic approach was associated with increased operating time but reduced blood loss and shorter hospital stays. However, both objective and subjective clinical outcomes should be considered when evaluating the procedure.
Conclusion
Significant progress has been made in applying robotic technology to the surgical treatment of a wide range of functional urology conditions. Since its introduction to the field over the past 15 years, robotic surgery has been adopted by early pioneers, but it has yet to become the mainstream approach in most settings. For all the clinical conditions discussed in this article, it is clear that the robotic approach needs to be studied in well-designed prospective trials to better establish its safety, clinical efficacy, and economic viability compared to laparoscopic and open approaches.
There are many potential advantages to using a robotic minimally invasive approach; however, this requires a high level of technical expertise and experience, especially for more complex procedures, particularly those involving the use of bowel or addressing complicated intra-abdominal and intra-pelvic environments, especially after previous surgeries.
Many of the robotic series in functional urology come from experts in robotic uro-oncological surgery. While technical proficiency with robotic surgery is crucial, it is not the only requirement. Surgeons must also have thorough training in functional urology, including in-depth knowledge of the conditions, their evaluation, management (including surgical principles), and postoperative care. While adapting traditional techniques for robotic surgery is practical, it is vital that key steps of the operation are not compromised. Looking ahead, structured training in robotics should be incorporated into functional urology training programmes.
---------
Read Part 1 of this article.