7. LOW SEXUAL DESIRE AND MALE HYPOACTIVE SEXUAL DESIRE DISORDER
7.1. Definition, classification and epidemiology
It has always been a challenge to define sexual desire properly because it has a complicated nature and it can be conceptualised in many different ways. According to the International Classification of Diseases 10th edition (ICD-10), lack or loss of sexual desire should be the principal problem and not other sexual problems accompanying it such as ED [857]. In the DSM-V, male hypoactive sexual desire disorder (HSDD) is defined as “the persistent or recurrent deficiency (or absence) of sexual or erotic thoughts or fantasies and desire for sexual activity”. The clinician makes the judgment of deficiency, taking into account factors that affect sexual functioning, such as age and general and socio-cultural contexts of the individual’s life [212]. According to the fourth International Consultation on Sexual Medicine (ICSM), the definition of male HSDD was proposed as a “persistent or recurrent deficiency or absence of sexual or erotic thoughts or fantasies and desire for sexual activity (clinical principle)” [858]. Although the exact prevalence of low sexual desire (LSD) is unknown, a prevalence of 4.7% was reported in a survey of a population-based sample of middle-aged German men (n = 12,646) [859].
7.2. Pathophysiology and risk factors
Several aetiological factors are considered to contribute to the pathophysiology of LSD. Levine proposed three components of sexual desire as drive (biological), motivation (psychological) and wish (cultural) [860]. However, it is believed that both in the surveys and clinical practice those three components are usually found interwoven [861].
7.2.1. Psychological aspects
The endorsement of negative thoughts during sexual intercourse (i.e., concerns about erection, lack of erotic thoughts, and restrictive attitudes toward sexuality) predicts LSD in men [862,863]. Furthermore, feeling shame during sexual intercourse, because of negative sexual thoughts (e.g., concern about achieving an erection), characterises men with LSD as opposed to women with the same condition [864]. Psychopathological symptoms stemming from a crisis context negatively impacted male sexual desire [355], as well. In addition, dyadic male sexual desire was best accounted for by sexual satisfaction [865]. It is worth noting that, despite LSD being less common in men than in women [858], it is the most frequent complaint in couples’ therapy [866]. Therefore, the role of relationship factors must be addressed. In addition, anxiety proneness has been associated with LSD in men and is expected to shift men’s attention from erotic cues to worrying thoughts, thereby decreasing sexual desire [867]. Finally, it is worth noting that current approaches focus on sexual desire discrepancies between partners; the focus on discrepancies rather than on the partner who presents low desire not only reduces stigma, but also provides new opportunities for managing desire in the relationship context [868].
7.2.2. Biological aspects
Testosterone seems to be essential for a man’s sexual desire; however, sexual desire does not directly relate to the circulating level of testosterone, especially in older men [869]. The biological and psychological components that take place in the pathophysiology of LSD are shown in Table 7.1 [861,870]. In addition to these factors, there is some speculation about the role of thyroid and oxytocin hormones [597,871].
Table 7.1: Common causes of low sexual desire in men [861,870]
| Androgen deficiency | Post-traumatic stress syndrome |
| Hyperprolactinaemia | Renal failure |
| Anger and anxiety | Coronary disease and heart failure |
| Depression | Ageing |
| Relationship conflict | HIV infection |
| Stroke | Body-building and eating disorders |
| Antidepressant therapy | Erectile dysfunction |
| Epilepsy | Prostatitis/chronic pelvic pain syndrome |
7.2.3. Risk factors
In an international survey aimed at estimating the prevalence and correlates of sexual problems in 13,882 women and 13,618 men from 29 countries (Global Study of Sexual Attitudes and Behaviours), risk factors for male LSD were age 60-69 and 70-80 years, poor overall health, vascular diseases, being a current smoker, belief that ageing reduces sex, divorce in the past 3 years, financial problems in the last 3 years, major depression, being worried about the future of a relationship and less than one sexual relation in a week [210]. In a recent study that determined the factors associated with LSD in a large sample of middle-aged German men, PE, ED, and lower urinary tract symptoms were associated with LSD [859]. In contrast, men having more than two children, higher frequency of solo masturbation, perceived importance of sexuality, and higher sexual self-esteem were less likely to have LSD [859].
7.3. Diagnostic work-up
7.3.1. Assessment questionnaires
Sexual Desire Inventory (SDI) evaluates different components influencing the development and expression of sexual desire [872]. This self-administered questionnaire consists of 14 questions that weigh the strength, frequency, and significance of an individual’s desire for sexual activity with others and by themselves. The SDI suggests that desire can be split into two categories: dyadic and solitary desire. While dyadic desire refers to “interest in or a wish to engage in sexual activity with another person and desire for sharing and intimacy with another”, solitary desire refers to “an interest in engaging in sexual behaviour by oneself and may involve a wish to refrain from intimacy and sharing with others” [872].
7.3.2. Physical examination and investigations
Similar to other forms of sexual dysfunctions, a thorough medical and sexual history must be obtained from men who complain of LSD. The depressive symptoms of the patients must be assessed [873] and relationship problems (e.g., conflict with the sexual partner) must be questioned. In the presence of accompanying symptoms suggestive of endocrinological problems, circulating total testosterone [874], prolactin [875] and thyroid hormones [597] levels can be evaluated.
7.4. Disease management
Treatment of LSD should be tailored according to the underlying aetiology.
7.4.1. Psychological intervention
Data on efficacy of psychological interventions for LSD are scarce. Accordingly, recommendations must be interpreted with caution. Psychological interventions with a focus on cognitive and behavioural strategies may be beneficial for LSD in men [359,876] (Figure 7.1). Mindfulness treatments may be a strong candidate, as well [876]. Since both members of a couple may experience age-related changes concurrently and interdependently, it could be helpful to address the sexual health needs of the ageing couple (including LSD) as a whole rather than treating the individual patient [877]. Indeed, psychologists are putting more emphasis on the concept of sexual desire discrepancy. Sexual desire discrepancy is often found in couples or partners, and mirror a natural part of life and partners’ dynamics. Clinical approaches based on this lens are less stigmatising as they consider the normal variations in sexual desire that occur throughout the lifespan. This intervention option targets couples distressed by sexual desire discrepancies rather than a single individual targeted as the one presenting low sexual desire [868].
Figure 7.1: Flow-diagram of psychological evaluation of patients with low sexual desire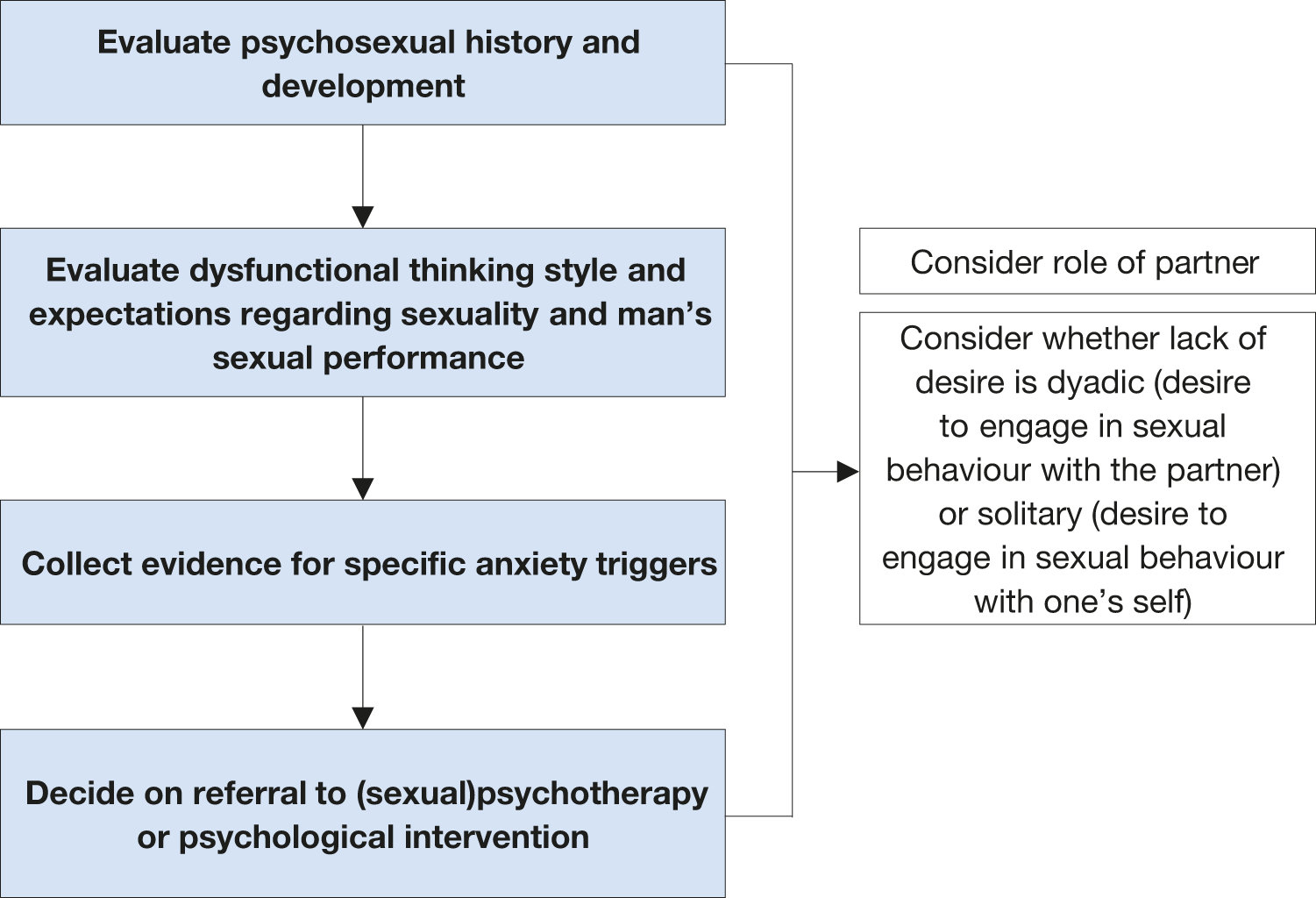
7.4.2. Pharmacotherapy
Low sexual desire secondary to low testosterone levels can be treated with different formulations of testosterone. The favourable effect of testosterone therapy on sexual motivation and the presence of sexual thoughts was shown in a meta-analysis [874]. The aim of treatment should be to reach the physiological range of testosterone (see section 3.3).
Hyperprolactinaemia can also cause LSD and one of the most relevant aetiological factors is prolactin-secreting pituitary adenomas. These adenomas can be easily diagnosed with MRI of the pituitary gland and can be treated with dopamine agonist agents [878]. The other accompanying endocrine disorders, such as hypothyroidism, hyperthyroidism and diabetes, should be treated accordingly.
Pharmacotherapy can also be used to treat major depression; however, it should be remembered that antidepressants may negatively affect sexual functioning; therefore, antidepressant compounds with less effect on sexual function should be chosen. Psychotherapy can increase the efficacy of pharmacotherapy, especially for patients whose LSD is due to depression [879].
7.5. Recommendations for the treatment of low sexual desire
| Recommendations | Strength rating |
| Perform the diagnosis and classification of low sexual desire (LSD) based on medical and sexual history, which could include validated questionnaires. | Weak |
| Include physical examination in the initial assessment of LSD to identify anatomical abnormalities that may be associated with LSD or other sexual dysfunctions, particularly erectile dysfunction. | Weak |
| Perform laboratory tests to rule out endocrine disorders. | Strong |
| Modulate chronic therapies which can negatively impact toward sexual desire. | Weak |
| Provide testosterone therapy if LSD is associated with signs and symptoms of testosterone deficiency. | Strong |